Testosterone and hemoglobin / hematocrit issues
and
The Vorck Ferritin Restoration Protocol for people on TRT
Debut: May 2021
Current document revision: June 2025
Ferritin Protocol version 4
As long as I am alive, this gets changed as new sources become available. Change log at bottom.
Goals
I will walk you through understanding why red blood cells, hemoglobin, and hematocrit all go up and ferritin goes down when on Testosterone or other anabolic steroids. I will discuss several myths about high hemoglobin and hematocrit and list the drugs and supplements that you might choose to use to keep these from rising.
In Section 2, I will walk you through why raising ferritin while on Testosterone is essentially impossible using the typical methods that work in people not on Testosterone, and I will show you a working protocol for raising your ferritin.
Notes before we start
• This guide is for people (yes, both men and women) on Testosterone Replacement Therapy. It is NOT for people with low iron, low hemoglobin anemia or iron disorders. If you have C282Y Hereditary Hemochromatosis do NOT do this (H63D is ok).
• Any topic that is in a dropdown is optional reading for the curious. It's not really central to the main topics of high hemoglobin and hematocrit or building ferritin.
• Do not use AI (not even the much celebrated ChatGPT) to summarize this page. As the author, I can assure you that AI models, including ChatGPT, Grok, Claude, and Llama get it REALLY wrong. Perplexity gave general answers like a kid that didn't do the reading.
• I don't take a position on donating. I will generally not tell you that you should or shouldn't (I will say that you have to if your HCT got to 60 though). I will tell you why the people who say that you never need to are often full of shit, though. I'll lay it all out and ultimately it's really your call. This is an options document to guide you in decision making.
• I recommend Nelson Vergil's community. I recommend Cortex Labs for video content. Avoid Reddit like it's cancer, it's a cesspool of misinformation. Sorry Redditors but you have people in there who don't read and don't know anything and are loud about it. Or just repeat nonsense.
Table of Contents, High Hemoglobin / Hematocrit
The One Minute Explanation for Physicians
Iron Basics in Blood, Oversimplified
High Hemoglobin and Hematocrit ("H&H") Explained
Popular Myths (includes "but altitude!" and "but Lance Armstrong!")
Managing With Phlebotomy (includes "do I do Power Red?")
Table of Contents, The Vorck TRT Ferritin Protocol
The Simple Version of the Protocol
The Detailed Version of the Protocol, with the science explained
What kind of iron you need to use for this protocol
Things that work against raising ferritin (only DURING the protocol)
Calculators (predicted E2 and DHT, pmol to ng/dL, E2 to TT ratio)
The One Minute Explanation for Physicians
Exogenous Testosterone increases EPO. It also acts directly on the bone marrow independently of EPO elevation.
Increased EPO causes the marrow to produce more RBCs.
When more RBCs are produced, more erythroferrone is also produced by erythroblasts.
When erythroferrone is produced, hepcidin is suppressed.
When hepcidin is suppressed, ferroportin in cells will allow stored iron (ferritin) to exit the cell very easily, re-bind to transferrin, and be used for hemoglobin. This will also prevent iron from being stored as ferritin normally in the first place.
Eighty percent of ferritin is stored in the liver. Retired RBCs are mostly stored as ferritin. Because of suppressed ferritin, the recycled iron also contributes to high hemoglobin.
This process does not always stop on its own. In some individuals, phlebotomy is the only way to keep it in check. Rusfertide, a synthetic hepcidin analogue, will solve this entire cyclic problem, but the drug has not yet been approved by the FDA.
Blood Basics
Generally speaking, these are the main components of blood:
1. Cellular components (~50% of total blood volume)
Red Blood Cells (RBCs) or erythrocytes (carry oxygen via hemoglobin and remove carbon dioxide).
Erythropoiesis is RBC production which takes place primarily in the bone marrow.
Erythroblasts: These are immature precursor cells in the bone marrow critical to RBC formation. They develop from hematopoietic stem cells and progress through stages (e.g., proerythroblasts, basophilic / polychromatic / orthochromatic erythroblasts). These become...
Reticulocytes: Erythroblasts lose their nuclei to become reticulocytes, which are released into the bloodstream and mature into RBCs within 1 to 2 days. These become...
Circulating RBCs: Mature RBCs circulate for ~120 days, carrying oxygen via hemoglobin to tissues and removing carbon dioxide. They are flexible, which allows efficient passage through capillaries.
Senescence and Destruction: After ~120 days, RBCs become less flexible and they are less able to navigate the spleen’s narrow sinusoids (tiny blood vessels). Trapped RBCs are phagocytosed (engulfed and broken down) by macrophages in the spleen ("splenic macrophages").
The iron from the RBCs that are destroyed is recovered and recycled.
Splenic macrophages break down hemoglobin into heme and globin. The heme is further degraded by the enzyme heme oxygenase into Iron (Fe2+, ferrous iron, or Fe++). Most of this iron (~65% to 80%) is released back into the bloodstream, bound to transferrin, the iron transport protein. This iron is delivered to the bone marrow for use in new RBC production.
White Blood Cells (WBCs) or leukocytes (your immune system made of Neutrophils, Lymphocytes, Monocytes, Eosinophils, Basophils). These cells cannot carry oxygen.
Platelets (Thrombocytes, for clotting).
2. Plasma (~50% of total blood volume)
The liquid part of blood, mostly water (about 90%), that transports cells, nutrients, and waste.
Contents of plasma include:
Water
Electrolytes (sodium, potassium, calcium, chloride, bicarbonate, and magnesium.)
Proteins (albumin, globulins, fibrinogen)
Nutrients (glucose, amino acids, lipids)
Waste products (urea, creatinine)
Gases (small amounts of O2, CO2)
Erythrocytosis: when the body makes too many Red Blood Cells (can be for various reasons).
Iron Basics in Blood, Oversimplified
Iron is an essential mineral that helps your body produce hemoglobin, the protein in red blood cells that carries oxygen throughout the body. There are two types of iron. Heme iron (Fe2+ or ferrous iron) comes from animal sources (like red meat) and is absorbed more efficiently by the body. Non-heme iron (Fe3+ or ferric iron) is found in plant-based foods (like beans and spinach) and is less readily absorbed, especially when consumed with foods that block iron uptake like calcium or tea.
Copper's Role in Iron Transport, oversimplified (because sometimes people ask about copper). Copper is chiefly used by the body to change the electron state of iron.
Ceruloplasmin serves as the primary carrier of copper in the blood. Not iron. It binds to copper ions, which are released from food in the digestive tract or released during the breakdown of old red blood cells. By binding to copper, ceruloplasmin ensures its safe transport through the bloodstream to different tissues and organs.
Besides its role in copper transport, ceruloplasmin also participates in iron metabolism. It has ferroxidase activity, which helps convert Fe3+ to Fe2+. As for ferritin, iron is oxidized by ferritin's own heavy chain for storage.
Hephaestin is primarily expressed in the enterocytes (cells lining the small intestine responsible for absorbing nutrients from food) and hephaestin regulates the release of iron into the bloodstream from the enterocytes via ferroportin. The mechanism by which hephaestin facilitates iron absorption involves its ability to oxidize ferrous iron (Fe2+) to ferric iron (Fe3+). Ferric iron is the form of iron that can be effectively transported across the enterocyte membrane and subsequently bound to transferrin, a protein that transports iron in the bloodstream.
Hepcidin and ferroportin allow iron to move. Not copper. Copper facilitates the move when hepcidin allows it.
Bottom line, copper does not play a role in this protocol.
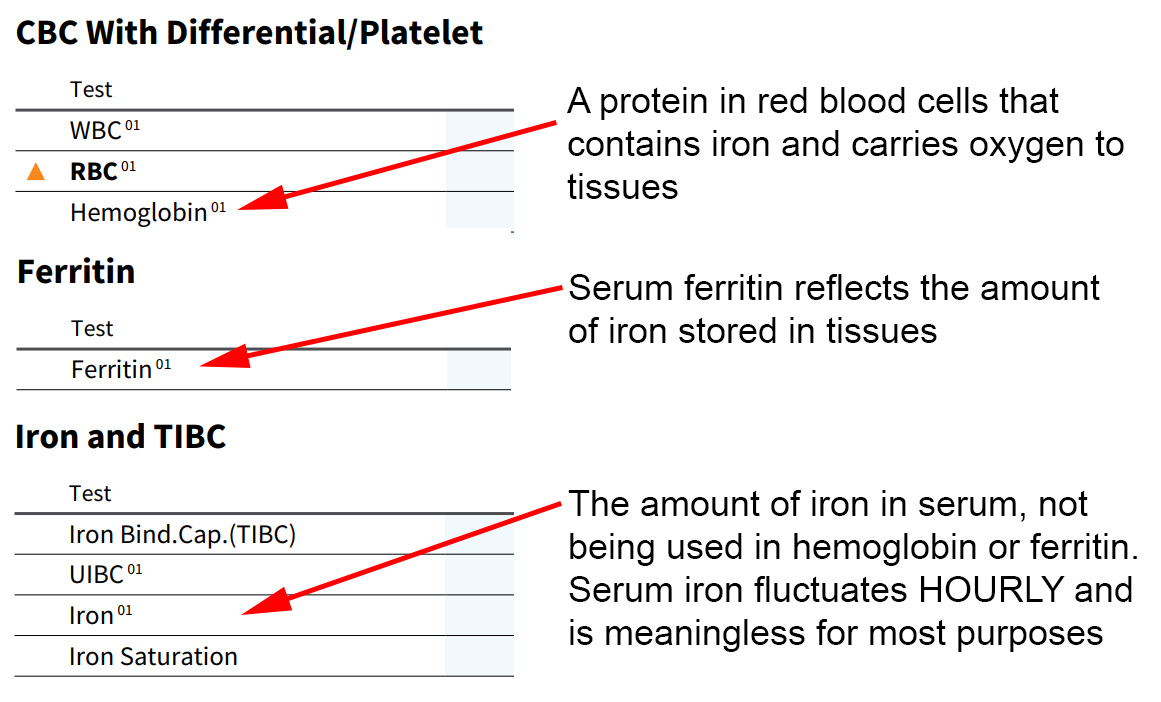
CBC (Complete Blood Count) is a common blood test that measures levels of red blood cells, white blood cells, hemoglobin, hematocrit, and platelets. It helps assess overall health and detect conditions like anemia, infection, or blood disorders. It is often called an FBC (Full Blood Count) in the UK, Australia, and sometimes Canada.
Hemoglobin (HGB): iron is a key component of hemoglobin, the protein in red blood cells that binds oxygen in the lungs and carries it to tissues throughout the body. Each hemoglobin molecule contains four iron atoms, which bind oxygen reversibly.
Hematocrit (HCT): measures the volume of red blood cells compared to the total blood volume (red blood cells and plasma). This is the one that is highly affected by hydration. It is a ratio, and by the way, donating plasma will increase HCT. This is the one that is highly affected by hydration. It is a ratio of RBCs to total blood volume, and by the way, donating plasma will increase HCT. A hematocrit of 50% means that 50% of your blood volume is made up of red blood cells, and the remaining 50% is plasma and other cells. If a person is severely dehydrated, hematocrit (and to a lesser extent, hemoglobin) will appear higher, and if the patient is fluid overloaded, they will be lower than their actual level.
Hydration is fundamentally necessary obviously but when people tell you that you can keep your RBCs and H&H low by drinking 4 liters of water per day, "that's not how any of this works." Hydration doesn't stop secondary erythrocytosis.
There is an old guideline that floats around that clinicians don't like using any more, but it's handy for us as it's true more often than not. It works like this: your hematocrit should be your hemoglobin multiplied by three. A hematocrit associated with a hemoglobin of 17 should be 54. If it's, say, 57, then you're probably dehydrated.
Myoglobin: iron is part of myoglobin, a protein in muscle cells that stores and releases oxygen for muscle activity, similar to hemoglobin but specific to muscles.
Ferritin: iron is stored in ferritin, a protein complex primarily in the liver, spleen, and bone marrow. Ferritin holds iron in a non-toxic molecular protein cage (it is not toxic like RCP / Morley Robbins people tell you). A little bit of ferritin exists in serum. The liver's cells (hepatocytes) hold 80% of the body's ferritin and it is released as needed for red blood cell and hemoglobin production and other processes. In a healthy normal person we want iron to go into hemoglobin as needed and into ferritin storage when hemoglobin is adequate. Ferritin in men tends to stay pretty constant for extended periods, weeks or even months, but blood donations and high levels of Testosterone even without blood donation will lower it. This will be discussed in greater detail later.
Transferrin: iron is transported in the blood by transferrin, a protein that binds iron and delivers it to cells.
Ferroportin: this is a cellular protein that allows iron to exit cells when ferroportin's level is high, and traps iron in cells when ferroportin's level is low. Ferroportin is controlled by hepcidin.
Erythropoietin (EPO): a hormone secreted mainly by the kidneys, this stimulates red blood cell production (erythropoiesis) in the bone marrow.
Hepcidin: this is a single-purpose hormone that is the master regulator of iron in the body. Hepcidin exists to:
• keep you from overdosing on iron by blocking absorption when appropriate
• keep cells from releasing iron when you're sick to avoid 'feeding' pathogens which feed on iron
It decides when iron can enter the body via absorption and whether iron can exit cells (it does both simultaneously). When hepcidin is high, it binds to ferroportin, trapping iron in the cells (AND it blocks absorption of iron in the gut at the exact same time). When hepcidin is low, there is nothing to bind to ferroportin, so iron exits cells easily (AND it allows absorption of iron in the gut at the exact same time). Hepcidin is a cellular "iron drain plug." There's more to hepcidin than that but for now, we're keeping it simple. Just remember: high hepcidin traps iron / blocks absorption. Low hepcidin lets iron flow out / allows absorption.
Since its purpose was discovered in 2001 by Dr. Tomas Ganz MD, the peptide hormone hepcidin has been identified as the principal regulator of iron availability in the body. [Source]
In order to regulate iron levels, the body responds to iron ingestion by increasing the amount of hepcidin. "Hepcidin levels rise in response to iron ... such that iron absorption and release are reduced." [Source] How does the body know you keep taking iron? The iron ingestion signaling process is outlined here.
[Read a paper by Ganz on his discovery of hepcidin 10 years later]
Erythroferrone: this is a single-purpose hormone that is the master regulator of hepcidin in the body. It is produced by immature Red Blood Cells. Lots of new RBCs means your erythroferrone level is high. When erythroferrone is high, hepcidin is low (and from the paragraph above -- when hepcidin is low, there is nothing to bind to ferroportin, so iron exits cells easily.)
The easiest way for me to describe the function of erythroferrone is to explain it this way: imagine you have lost a lot of blood. You would want the iron in your body available for use in hemoglobin to carry oxygen. You would not want your body to store iron in ferritin. When you lose blood, your body makes new RBCs. These new RBCs produce Erythroferrone. Erythroferrone pushes hepcidin down. Low hepcidin lets iron flow out of cells for use in hemoglobin, ensuring that iron cannot be stored so that it can be used to make hemoglobin to carry oxygen and save you from dying after blood loss. The term for this is "iron mobilization for increased erythropoiesis."
A question about erythroferrone that I want you to think about: what would happen if erythroferrone were somehow high, but you weren't bleeding? What would your body do? It would draw iron from ferritin for use in hemoglobin -- even when you don't need it to.
(Serum) Iron: this is the amount of iron waiting for transport to cells. It changes hourly (yes, really) based on what you eat and is NOT meaningful for our purposes. It is used in diagnostic tests with other metrics for evaluating blood disorders like hemochromatosis. [Read about iron]
In the TRT world, many men are in the bad habit of saying "my iron is" [high or low] when they could mean hemoglobin, serum iron, or ferritin.
In the human body, Fe2+ (ferrous iron, which could be written Fe++) and Fe3+ (ferric iron, which could be written Fe+++) are two forms of iron that play key roles in metabolism and transport.
Fe2+ (ferrous) is the reduced form and is the type of iron that is absorbed through the intestine. It is also the form that binds oxygen in hemoglobin.
Fe3+ (ferric) is the oxidized form and is less easily absorbed. Dietary iron (especially non-heme) is often in the Fe3+ form and must be reduced to Fe2+ before it can enter intestinal cells. Serum iron (the iron measured in blood tests, bound to transferrin) is mostly in the Fe3+ (ferric) form, as this is the form transferrin carries safely in the bloodstream. Ferritin stores iron in this form inside cells.
The conversion of Fe2+ (ferrous iron) to Fe3+ (ferric iron) is called oxidation. This process involves the loss of one electron from the Fe2+ ion.
The conversion of Fe3+ (ferric iron) to Fe2+ (ferrous iron) is called ferroreduction. This process involves the gain of one electron by the Fe3+ ion.
Inside the body:
Dietary non-heme iron is typically in the Fe3+ (ferric) form and must be reduced to Fe2+ by enzymes like duodenal cytochrome B (Dcytb) on the surface of intestinal cells for absorption.
Once inside the cell, iron must eventually be exported into the bloodstream. But in the blood, iron needs to be in the Fe3+ form to bind to transferrin, the transport protein.
This re-oxidation of Fe2+ to Fe3+ is carried out by hephaestin (in enterocytes) and ceruloplasmin (in the blood), both of which are copper-dependent enzymes.
The items of importance on a Complete Blood Count
Other Terminology
TRT: Testosterone Replacement Therapy. In our context, this can include any androgen via injection. Delivery methods like oral, buccal, gels, creams, and the like are not associated with high levels of RBCs.
Testosterone Proprionate (first synthesized in 1936 and marketed for medical use in 1937, was the first ester out of the gate and due to its short half life is typically not associated with SE.
The common anabolics with longer half lives like Cypionate (synthesized in 1951, marketed by Upjohn for medical use in 1951), and Enanthate (synthesized in 1952, marketed by Squibb for medical use in 1954) were created for long lasting TRT.
The FDA approval process as we know it today was formalized after the 1962 Kefauver-Harris Amendments, which required drugs to demonstrate both safety and efficacy. Since testosterone cypionate and enanthate were introduced before this, their initial modern FDA approval was in 1979.
Interestingly, anabolics like Nandrolone (synthesized in 1950, licensed for medical use in 1959) and Oxandrolone (synthesized in 1962, licensed for medical use in 1964) were created for other purposes, including raising hematocrit. The erythropoietic profiles of these drugs were studied in the context of seeking the best treatment for dialysis patients in the 1960s.
Phlebotomy: Any kind of controlled monitored bloodletting including donating blood.
Clinicians: MDs, DOs, Psychiatrists, Physician Assistants, anyone who is authorized to prescribe pharmaceuticals.
Hepatocytes: these are the main functional cells of the liver and store 80% of the body's ferritin.
Hypotension, Hypertension: Low and high blood pressure, respectively. More on normal BP below.
Chelation: Chelation is a chemical process in which a substance (called a chelator) binds to a metal ion to form a stable complex, making the metal easier to remove from the body, often through excretion in urine. In our world, anything that chelates iron can be useful for lowering H&H, but this also comes at a price of lowering ferritin as well. More on this further below.
Normal Blood Lab Values
The normal lab ranges in human beings are based on population averages that were set decades ago. The common normal ranges that we are concerned with are:
Hematocrit (HCT) as a percent
Men: 42 - 52* (some labs use 50, some 54)
Women: 37 - 47
Hemoglobin (HGB) in g/dL
Men: 13.5 - 18.0*
Women: 12.5 - 16.0
Red Blood Cells (RBCs) x10E6/uL
Men: 4.7 - 6.0
Women: 4.2 - 5.4
Platelets x10E3/uL
Men: 150 - 450
Women: 150 - 450
*18 x 3 = 54. Some guidelines say HGB of 18 or HCT of 52 needs phlebotomy.
HCT should be calculated directly but some labs derive it using one of two formulas:
Hct = (0.0485 × concentration of hemoglobin in mmol/L + 0.0083) × 100 or
Hct = MCV × RBC × 0.1.
More reading on lab values is available here.
Get before starting:
• LH
• FSH
• DHEA-S
• Cortisol
• Thyroid Panel
Get before and after starting:
• CBC
• Total Testosterone
• Free Testosterone
• SHBG
• Estradiol (specify “sensitive” assay for males)
• Prolactin
• PSA
• Vitamin D
• Ferritin
• Metabolic Panel
• Lipid Profile
You will get a CBC as part of the test anyway; note CBC values of HCT, HGB, RBC. An iron panel isn't necessary, but some people like to see Transferrin Saturation.
Normal Blood Pressure
From the Merck Manual page on BP
In adults, doctors classify blood pressure as:
Normal: Less than 120 / 80
Elevated: 120–129 systolic AND less than 80 diastolic
Stage 1 high blood pressure: 130–139 systolic OR 80-89 diastolic
Stage 2 high blood pressure: 140 or more systolic OR 90 or more diastolic
After many years, high blood pressure causes serious problems, such as heart attack, heart failure, stroke, or kidney damage.
We will be discussing some blood pressure drugs later in ways to reduce high H&H.
High Hemoglobin and Hematocrit ("H&H") Explained
What exactly is the issue with Testosterone raising hemoglobin and hematocrit?
Men (and some non-menstruating women) on TRT sometimes develop a problem with erythrocytosis, making too many RBCs, which raises hematocrit (HCT) by skewing the ratio of red cells to serum.
Primary Erythrocytosis refers to conditions where the bone marrow produces excessive RBCs due to intrinsic marrow abnormalities. Secondary Erythrocytosis happens when high RBCs are due to an external cause like hypoxia or elevated erythropoietin (EPO).
Testosterone drives what is known as "secondary erythrocytosis" (SE). This often first shows up in the three month lab work that most clinicians order for patients on TRT.
In older research literature, this issue was sometimes referred to as Polycythemia or Polycythemia Vera. PV is actually a separate condition.
Polycythemia is simply a dated term. If you see it, don't freak out. Physicians who are older may have had medical training on androgen replacement that conflated the two, something older textbooks actually do. Harrison’s Principles of Internal Medicine and Williams Hematology began switching from the term polycythemia to erythrocytosis in 2000.
Because of this, some physicians may recommend donating blood when hematocrit gets above 45. This "keep it 45" guidance was appropriate for Polycythemia Vera ("PV") not for secondary erythrocytosis ("SE"). Yes, there is a difference between just Polycythemia and Polycythemia Vera. When you see the word Polycythemia without the "vera" in medical literature, it absolutely means erythrocytosis. It's just an older term.
Some guys mindlessly parrot "Erythrocytosis and Polycythemia are different things!" By this, they mean that since PV requires bloodletting, and SE and PV are different, then bloodletting isn't necessary for SE. Saying SE doesn’t need phlebotomy because it’s not PV is like saying a forest fire caused by lightning doesn’t need water because it’s different from a fire started by a campfire.
The issues related to high H&H relate to stroke (debatable, read on about why), cardiac problems (also debatable, read on about why), and temporary pulmonary hypertension (OMG they didn't mention that in that YT video!)
What drives Testosterone to make Red Blood Cells?
There are multiple contributors to erythrocytosis while on TRT.

[Source from 2018]
Testosterone acts directly on the bone marrow independently of EPO elevation. [Source, source]
The largest contributor by far of increased RBCs is the stimulation of erythropoietin.
When you inject Testosterone, it will be bound to Sex Hormone Binding Globulin (SHBG), to Albumin, and the remainder is unbound and termed "Free."
We have known since 2005 that Testosterone bound to SHBG is transported into cells expressing Megalin, a cellular surface protein. (20 years later we still have people saying SHBG bound Testosterone isn't used. Some myths cannot die.) [Source]
The human body has by far the absolute highest concentration of cells expressing Megalin in the Proximal Tubule Epithelial Cells of the kidney. It's like the majority of Testosterone is essentially made for going right to the kidneys and stimulating EPO.
"Testosterone stimulates red blood cell production (erythropoiesis) by stimulating erythropoietin (EPO) and recalibrating the set point of EPO in relation to hemoglobin and by increasing iron utilization for erythropoiesis.
The 7%-10% increase in hemoglobin and hematocrit, respectively, with testosterone administration was associated with significantly increased erythropoietin (EPO) levels and decreased ferritin and hepcidin levels at 1 and 3 months. (Ferritin and hepcidin are explained further down.) At 6 months, EPO and hepcidin levels returned toward baseline in spite of continued testosterone administration, but EPO levels remained nonsuppressed even though elevated hemoglobin and hematocrit higher than at baseline, suggesting a new set point." [Source]
The study on the EPO setpoint is from 2014, the same year erythroferrone was discovered, which is the missing link here and the reason the connection between RBCs and hepcidin is vague in the link. This link describes how erythroferrone crushes hepcidin.
A mouse study was conducted that same year which noted the "Testosterone crushes hepcidin" effect, but these researchers were also obviously unaware of erythroferrone. [Source] Incredibly, the same team of researchers were still unaware of EPO and erythroferrone 5 years later, sadly, illustrating what happens when you're in a bubble. [Source]
Think about how information propagates. How would you find articles to read about some unknown thing on the Internet if you didn't know the thing existed in the first place? Only young hematologists would know how this process works, and the only hematologists that have patients on TRT would be those ordering phlebotomy after screening for Polycythemia Vera. Sure, doctors know about TRT and erythrocytosis but how many would know about all the pieces, especially if the last piece of the puzzle was only discovered in 2014?
Remembering what we've learned from earlier, let's put it all together in one sentence:
Testosterone binds to SHBG, is transported into kidney cells, which increases erythropoietin (EPO), which causes more erythroblasts (immature RBCs) to be produced, which secrete erythroferrone, a hormone which suppresses hepcidin, which in turn causes iron to flow out of cells and into hemoglobin.
This mechanism is both starting a fire (more EPO, more RBCs) and adding gas (mobilize iron for those RBCs) at the same time.
In terms of EPO, the research does say that this tends to normalize after 6 months to a year on TRT. I and others have been on TRT for decades and I still have to donate though. Eventually normalizing is not guaranteed.
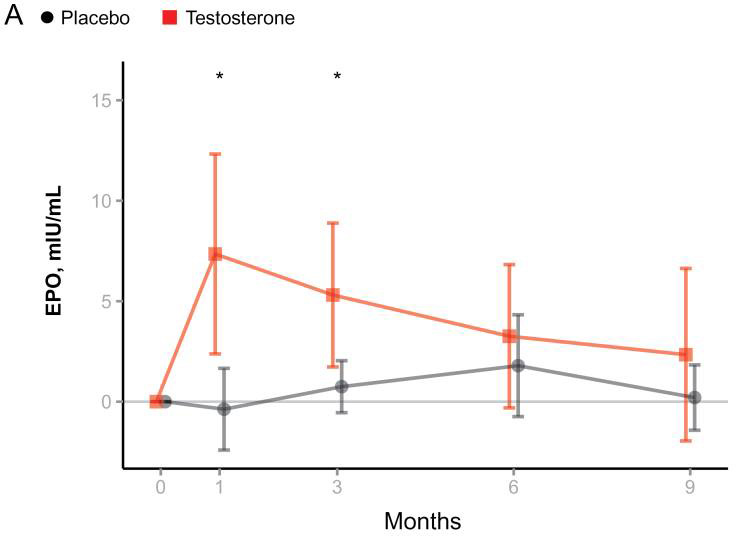
The subjects in this EPO setpoint study did not go above a TT of 500! You can imagine men who keep higher levels of Test. The study, linked right below, has similar graphs showing major impacts on hepcidin and ferritin as well.
TRT alters iron metabolism as well: Testosterone Enanthate at 125 mg per week reduced serum ferritin 32% within 3 months of treatment initiation without altering iron, transferrin, or transferrin saturation. (Hepcidin was suppressed 57%). [Source]
THIS MEANS TRT ITSELF CAN DEPLETE FERRITIN OVER TIME WITHOUT ANY BLOOD DONATION.
Kidney function varies among men of course, but I stopped for 21 days just to see what would happen to my EPO. 21.9 to 9.9. I picked 21 days randomly. At this point I had been injecting for 20 years. I moved up from 160mg to 210mg per week at age 50 to get to the same amount of Total (my personal ideal is 750 to 800ng/dL).

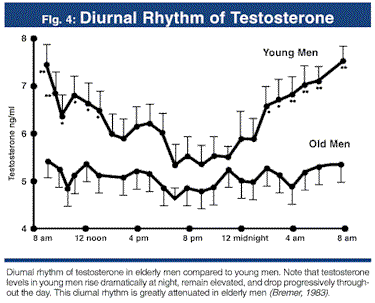
How come this doesn't happen to young men with presumably high Testosterone?
Because their Test levels, even if high, vary throughout the day. [Source] When you're on TRT, your Total level is steady high and only your Free varies a very little over the course of the day. Young guys with naturally high Test levels are not at that 900 level 24/7. Gel and Natesto do not have high incidences of HCT issues and that's because they are TRT methods where levels go up and down quickly over the course of a single day. Not the case on injections. Here's a study that used 25 year old males. [Study]
The problem of high hemoglobin/hematocrit is not always due to Testosterone
There are multiple other reasons that H&H can be elevated besides TRT.
Polycythemia vera (PV) is a rare blood condition, technically classified as a cancer, where your body makes too many red blood cells. PV happens because of a mutation in bone marrow -- specifically the JAK2 gene. Doctors usually find it initially with a high RBC count on your CBC blood test. A medical history is taken to see if your high RBC count might be from something else, like smoking or sleep apnea (list of causes is below). If nothing in your history indicates a reason, the JAK2 test is then given. Phlebotomy is usually the ideal way to manage PV, but drugs are being developed to manage it as well, discussed below. A smart doctor also orders an EPO test at the same time as the JAK2 test, because if the JAK2 is negative for a mutation, the EPO test can help in determining what other cause might be the problem. In PV, the EPO level is actually normal or even LOW.
Primary Erythrocytosis (Not-PV!) is also rare. It can be caused by genetic mutations leading to increased erythropoietin (EPO) sensitivity or dysregulated oxygen sensing. Examples include mutations in the EPOR (erythropoietin receptor) gene or genes affecting the hypoxia pathway, such as VHL, HIF2A (EPAS1), or PHD2.
Secondary Erythrocytosis (SE) is actually quite common. Generally, EPO levels are low in primary causes, and elevated in secondary causes. Increases in EPO can come from:
The common causes of SE
Smoking (a hypoxic process)
Sleep apnea (a hypoxic process)
Testosterone use
Uterine fibroids, PCOS, hyperandrogenism
The less common causes
Chronic obstructive pulmonary disease (COPD) (a hypoxic process)
High altitude living or exposure (a hypoxic process)
Carbon monoxide exposure (leaky furnaces count) (a hypoxic process)
Elevated levels of Growth Hormone or IGF-1
The rare causes
Right-to-left cardiac shunts (heart disease)
Renal tumors that produce EPO
Dehydration (yes, this is really a rare cause)
Reduced plasma volume due to severe burns or diuretic overdose
Common causes of secondary erythrocytosis include a handful of things other than using Testosterone.
"In humans and other mammals, hypoxia modulates EPO levels by increasing expression of the EPO gene." [Source]
Simplified: snoring and smoking also increase RBCs. You may not even be aware of apnea, as the problem is low Oxygen saturation while you sleep. [Source, source] The best avenue is getting a sleep study as quickly as possible and getting on a CPAP or APAP machine. Unfortunately, these devices are by prescription only per FDA rules. Yes, you need the government's permission to breathe at night. Current practice favors fixing sleep apnea before TRT if hematocrit is over 52. [Source]
What is thought to be the risk of a high hemoglobin/hematocrit?
The risk, as conventional wisdom goes, is that SE could cause blood clots, heart attacks, and strokes: "Much of the concern surrounding increases in blood viscosity resulting from increased red blood cell mass centers on the potential increased risk for venous thromboembolism (VTE) (symptoms), myocardial infarction (MI), and cerebrovascular accidents (CVA) (symptoms)." [Source] A U-shaped relationship exists between haematocrit and mortality shown in a large prospective cohort study: [Source] Hypertension is also a risk, very common on TRT. [Source]
Note that quote didn't have the word "platelets" in it, by the way. Hyperviscosity due to increased red cell mass is a problem in and of itself.
Post 2010 research is casting some doubt on the absolute risk of stroke and heart attack:
"No evidence exists that a high hematocrit is harmful and a direct cause of thrombosis; in addition, many conditions that lead to a very high hematocrit are not associated with thromboses." [Source]
Large scale studies show no association between TRT and thromboembolism. The first study done in 2015 is here: [Source] A 2018 study that included six Randomized Controlled Trials (n = 2,236) and five observational studies (n = 1,249,640) is here: [Source] "There was no evidence of a statistically significant association between [venous thromboembolism] and testosterone."
"Several lines of evidence suggest that an isolated elevation in hematocrit does not, per se, lead to thrombosis. [...] Coronary blood flow is decreased in secondary erythrocytosis, but there is equivocal evidence as to whether the risk of coronary thrombosis is increased in patients with a high hematocrit." [Source]
"Increased Hct is associated with increased blood viscosity, reduced venous return and increased platelet adhesiveness. [...] Based on Endocrine Society Clinical Practice Guidelines, once a Hct > 54% is reached, TTh should either be discontinued, or therapeutic phlebotomy offered to reduce the risk of potential future thromboembolic events." However, "...few data support an increased risk of CV events resulting from testosterone-induced erythrocytosis." [Source]
None of these studies controlled for phlebotomy or blood donation.
I'll repeat that: none of these studies controlled for phlebotomy or blood donation. In other words, these high hematocrit studies were done on Testosterone users and some of those men in the studies were giving blood. So they showed that guys on TRT, some of whom gave blood, didn't have strokes. Probably because they were giving blood. (Hey, don't shoot the messenger here.)
"But platelets!" RBC values like MCV and MPV, not just raw platelet count, factor into risk. Also, high HCT (heart risk) versus high PLT (brain risk) are considered here in the Copenhagen study separately. Read this one carefully and scroll to 4, Discussion.
"Neither high platelet count nor high hematocrit was associated with risk of venous thromboembolism. When excluding individuals with myeloproliferative neoplasia (PV) from the main analyses, results on risk of thrombosis were similar. In this prospective study, high platelet counts were associated with 1.8-fold risk of arterial thrombosis in the brain, whereas high hematocrit was associated with 1.5-fold risk of arterial thrombosis in the heart."
So the science does NOT simply say that you do or don't need to donate.
If you become symptomatic with flushed red skin and shortness of breath, are you just going to deal with that and not donate? (This is the biggest problem I have with the Rouzier video, by the way.) High hematocrit levels make the blood more viscous (thicker). This increased viscosity can make it more difficult for the heart to pump blood through the pulmonary arteries, leading to higher pressure in these vessels, meaning having an HCT of 60 can mean you're tired all the time because you have (temporary) pulmonary hypertension until it's relieved with phlebotomy.
What are the symptoms of a high hematocrit?
Not everyone experiences them at an HCT of 50. Hypertension, itching and tingling in your extremities, headaches, getting winded more easily. The hypertension is from both EPO and more RBCs.
I have some pressure below my bottom left rib...
Your body recycles the iron from RBCs when the RBCs are filtered and "retired" in your spleen (the liver playes a role here as well). When your RBCs get too high, you can experience splenomegaly, an enlarged spleen, which feels like slight pressure below the lowest left rib. This is transient and not harmful, in and of itself. A doc can check it by feel (in less than one minute) or CT scan. It can be a warning sign for people not on TRT though. [Further spleen size reading]
(I would source this, but it appears in the research literature as an effect of PV, and explaining that it's really just the Red Cells as opposed to WBCs and platelets would be another 6 paragraphs. If you ask your doc if erythrocytosis can cause splenomegaly with RBCs over 6.5, he will say 'yes,' I assure you.)
Popular Myths
I heard that high HCT on TRT is the same as living at altitude, and those people don't donate.
Because the average male HCT at elevation in Bolivia is 52.
Healthy persons living at 4,000 meters (13,100 feet) in Bolivia:
hematocrit (HCT)
Men: 45-61 (average 52.7%)
Women: 41-56 (average 48.3%)
hemoglobin (HGB)
Men: 13-21 g/dL (average 17.3)
Women: 12-19 (average 15.8)
[Source] Comparison: Breckenridge, CO is 9,600 ft. Santa Fe, NM is 7,200 ft.
People at elevation do not all have HCT's of 60 if the average is 52. In addition, some Andeans do have altitude sickness and produce massive amounts of Red Blood Cells. [Source]
Also, there aren't medical centers for people to donate blood. Just because they don't have Starbucks there, does that mean they must not drink coffee?
The whole altitude issue is vastly more complex than people summarize it to be. [Explanation] TL;DR - doing TRT doesn't make you exactly like a Peruvian who lives his whole life at 30,000 feet. They literally have evolutionary adaptations (explained in these links). [Source]
High elevation and high RBCs occurred where there was a higher T to E2 ratio contributing to the erythrocytosis. Study on ratio. Androgens may be linked to mountain sickness [Study]
People at elevation reach a plateau, because the mechanism of their erythrocytosis is activation of HIF which increases EPO a much smaller amount than being on TRT. On TRT, Testosterone has a direct stimulation effect on EPO so in many users HCT just keeps going up and won't stabilize. That's just one 'for instance'. It is SUCH A LENGTHY TOPIC to address and guys and even docs on YT just blithely ignore the biology. Exactly ZERO YT docs mention this. Hypoxia-inducible factor was discovered in 1992. Are the older docs simply out of date?
Testosterone acts directly on the bone marrow independently of EPO elevation. [Source, source] In the first study, they actually measured EPO output and the dose of testosterone and the hemoglobin. It's fairly stable, they increase testosterone, EPO is still stable, but hemoglobin still goes up because testosterone is directly acting on the bone marrow.
I heard that high HCT on TRT just means I'm like Lance Armstrong, an endurance athlete.
Lance Armstrong's hematocrit during competititons never went above 50. This is documented in various places [source] [source] and he himself has noted it in interviews. [source] In the video, note what he says about Everest climbers. Do you really think there are people LIVING on top of Everest with an HCT of 70? Living there. NO ONE lives on top of Everest. And do you really think performance athletes let their HCT climb and climb and climb to the point where they suffer pulmonary hypertension? That's what will happen on TRT, because the effect of EPO isn't going to just magically stop.
"But maybe he was lying!"
OK but he said he didn't go above 50 in the same interview where he admitted cheating. Why would he tell the truth about cheating but lie about his hematocrit?!
I heard that Testosterone dilates blood vessels because of nitric oxide.
Low testosterone causes endothelial issues. [Source] Nitric oxide is mediated in part by testosterone. [Source] What I am not clear on, and cannot find research on, is whether running a Total from 500 to over 1,200 eliminates any risks from high hematocrit. If it worked that way, wouldn't a higher Total cause LOW blood pressure? And yet it doesn't seem to; high blood pressure is common on TRT. If you have a source showing higher T means more vessel dilation, please send it to me.
Managing Without Phlebotomy
Should I reduce my Testosterone dose?
Here is a study of 7,000 men on injected TRT whose HCT level normalized between 605–1051 ng/dL.There were 60 (sixty) of them. That's .86% or LESS THAN ONE PERCENT. Do you want to go into the 500s? We still see guys with erythrocytosis with Total Testosterone levels in the 400s too. At what point do you stop lowering the dose? Why not use gel or Natesto instead? You won't have high hematocrit as these mechanisms aren't associated with high HCT.
Could injecting subcutaneously instead of IM help?
It may possibly help you or delay the inevitable. SC dosing using a subcutaneous testosterone enanthate autoinjector (like Xyosted) "was associated with 41% and 26.5% lower post-therapy increases HCT and Estradiol levels respectively when compared to IM injections." [Source] The study compared the same amount of Testosterone used both IM and SC, and the study's numbers show an average TT of 536.4 and HCT of 48.4 in IM users and an average TT of 552.5 and HCT of 46.3 in SC injection users. Overall we are looking at 2 points lower HCT with SC dosing. That's significant in the world of TRT.
Could switching to gel, cream, buccal, nasal, or oral undecanoate help?
A lot of men report no rise in H&H when on these delivery systems because Testosterone is able to fall rapidly during the day.
Could different Testosterone dosing frequency help?
Studies that compare different TRT delivery methods show injection correlates to the highest frequency level of Erythrocytosis compared to gel or pellets. [Source] The problem is that the studies compare once weekly dosing of Enanthate and Cypionate (pictured below). That's not steady delivery of TRT; once weekly means huge peaks and troughs.

Link to original
Link to the study I got this from (see page 421 of the PDF)
As such, when trying to figure out SE, comparisons between gel, oral undecanoate, IM undecanoate, pellets, and shots don't really have much value. All it shows is that (1) lower doses of TRT (2) taken daily are less likely to cause SE. Note the numbers -- both size of dose AND frequency are factors. If you don't want to give up your dose size, split it into more frequent doses first. That might eliminate your SE.
Exercise could potentially help. [Source] But some exercise raises EPO.
Can I take any drug or supplement instead of donating blood?
The answer is a qualified maybe. Some of the drugs and supplements below don't work, I just discuss ALL of them that get mentioned in TRT circules.
Blood Pressure Drugs
Angiotensin II Receptor Blockers or "ARBs." (Telmisartan etc). This class of drug is used to lower blood pressure. Telmisartan works by blocking the angiotensin II type 1 receptor (AT1R). Angiotensin II plays a role in erythropoiesis by indirectly influencing erythropoietin (EPO) production, especially in the kidneys. Someone in a forum said these drugs give you ED. Not true. Many Telmisartan users in forums have reported that at 40mg and above, their need to donate slowed significantly or stopped. Losartan appears to work as well in some users. Losartan 20 didn't work for me, Telmisartan 40 did.
Angiotensin-Converting Enzyme inhibitors. (Lisinopril etc). This class of drug is used to lower blood pressure."Various mechanisms have been offered to explain why ACE inhibitors might affect the response to erythropoietin." [Alt link]
Other BP drug: Amlodipine lowers HCT. [Source]
Beetroot. It has a small amount of iron. Enough to raise H&H? In the amount we would take probably not. Beetroot powder boosts NO via nitrate conversion and enhances aerobic performance by improving oxygen efficiency and delaying fatigue. Increases plasma nitrate/nitrite levels by 50-100%, directly enhancing NO. Produces a more immediate and robust increase in NO due to its high nitrate content. L-citrulline provides a slower, sustained NO boost via L-arginine. 6 to 8 hours half life. Recommended dose is 6 to 12 grams (not mg). Further reading.
L-Citrulline. This converts to Argenine which offers a great NO boost and helps with exercise fatigue. Citrulline can keep H&H stable. It does this by mildly interfering with NCOA4 which prevents release of iron from ferritin. It is best used in combination with an ARB like Telmisartan. When you take Argenine it is rapidly metabolized by the liver, so it's not as beneficial as taking L-Cit which is an Argenine precursor. During high-intensity exercise or prolonged physical activity, muscles break down amino acids, producing ammonia as a byproduct. Ammonia is also generated during protein metabolism in the liver. Elevated ammonia levels in the blood and muscles increases fatigue by impairing muscle contraction and energy production. L-citrulline plays a key role in the urea cycle, which detoxifies ammonia; beetroot does not do this. Usually exercise does NOT outpace the body's ability to process the ammonia, but I've seen the fitness routines of some fo you guys so I know that's not always true. 2 hour half life. Recommended dose is 6 to 8 grams (not mg). Further reading.
FWIW Beetroot and L-Citrulline have independent mechanisms and can be taken together.
Chelating Agents
Simply speaking, these bind to iron and cause you to excrete it in feces and urine. Since your RBCs are still going to go up on TRT, chelating iron just forces your body to take iron from recycled RBCs and ferritin. This can make someone not on TRT anemic. It keeps ferritin from going up in people on TRT. [Discussion]
Grapefruit. This chelates iron, which lowers H&H and ferritn. This was an unexpected finding in a study on eating grapefruit. Many men do have success, despite that the study’s results have never been replicated. Naringin is the presumed agent in the Grapefruit, but it hasn’t even been confirmed. The study used whole fruit. Note that because Grapefruit is a CYP3A4 inhibitor, it can cause other drugs to stay in your body much longer, potentially very serious for some classes of drug. This is a discussion of the drugs affected. Some guys have tried and had success with grapefruit seed extract which is different than Naringen. (Grape seed is different from grapefruit seed by the way. That seems obvious when you read it here but it's easy to make the mistake when you're shopping and distracted. By the way, the aromatase inhibiting effect of grape seed has never been confirmed in humans.) Here is a mouse study on its potency. [Source]
Naringen. See grapefruit above.
Quercetin. Stronger chelator than naringen. Also causes issues with drugs that use the CYP3A4 pathway.
These both interfere with Cytochrome P450 3A4 (abbreviated CYP3A4). This is a liver enzyme that metabolizes many different drugs, so that they can be removed from the body.
Interfering with this enzyme will lengthen the half life of a drug that uses the CYP3A4 metabolic pathway, making the drug last longer. Common examples include Tadalafil (Cialis) and Sildenafil (Viagra), Cabergoline, Atorvastatin (Lipitor), Amlodipine (Norvasc), and Alprazolam (Xanax). To a lesser degree: Arimidex, Exemestane.
Read a paper on quercetin and it's other uses.
Hemoflow. This is Quercetin and Nattokinase. It will deplete ferritin. Obviously the idea is to lower iron systemically and use Nattokinase to affect blood viscosity.
Turmeric. Chelating agent. In high doses of 500mg daily, it will keep iron low and therefore hemoglobin low. It can make normies anemic and prevent ferritin from rising. [Source]
Curcumin. Same as Turmeric. It lowers hepcidin for as much as 24 hours post ingestion. [Source]
IP-6. Chelating agent. It chelates iron and will keep your hematocrit low over time by keeping you iron deficient. IP-6 binds with iron in the gastrointestinal tract so that's also going to keep you from raising ferritin. [Source]
Milk Thistle (silymarin). Chelating agent. [Source]
Miscellaneous Drugs
5α-Reductase inhibitors. These reduce DHT. Remember at the top of the page, that box showing the different factors that contribute to rising red cells? These drugs reduce DHT, and that might help a bit, but then again, LOTS of guys on TRT use drugs in this class like Cialis, and still get erythrocytosis. Don't expect a miracle. Note the study didn't even track EPO levels. That actually makes the study next to worthless. We don't know the Total and Free Test levels the men took, all they measure was DHT. But for what it's worth, here's the study anyway. [Source]
Finasteride. (Maybe). Don't take this for managing SE. That would be foolish. I am including it for completeness' sake. One study showed an impact on H&H [Source] and one study showed no difference. [Source]
Arimidex. Don't go overdosing and make me regret adding this, guys. This drug reduces Estradiol. Estrogen can affects hematopoietic stem cells, which are the precursor cells for erythroblasts. Estrogen receptors are present on hematopoietic stem cells, and estrogen signaling can impact their proliferation and differentiation. This can indirectly influence the production of erythroblasts. [Source] The amounts of Arimidex TRT users take doesn't significantly lessen erythrocytosis. By the way, while I'm at it, Estrogen also suppresses hepcidin.
Pentoxifylline. Don't take this, I am including it for completeness' sake. This drug works by reducing blood viscosity and by decreasing the potential for platelet aggregation and thrombus formation (decreases plasma fibrinogen concentrations). [Source]
Hydroxyurea. Don't take this, I am including it for completeness' sake. Hydroxyurea is used to treat PV (and some other diseases like Sickle Cell) and works by "inhibit[ing] the formation of DNA by blocking an enzyme known as ribonucleotide reductase. This results in the decreased ability of the bone marrow to produce red blood cells."
Unfortunately, Hydroxyurea lowers everything -- erythrocyte [Red Blood Cell], leukocyte [White Blood Cell], and platelet counts. Since PV and SE are different, you won’t find a physician who will prescribe this drug to you. Additionally, although it appears not to show the effect in low doses, taking Hydroxyurea has been associated with causing leukemia, one of the diseases it’s designed to treat.
Miscellaneous Drugs, Not Yet Approved
Divesiran. Silences TMPRSS6 gene via RNA interference, elevating hepcidin. Not yet approved. Currently in Phase III trials. (Although PV isn't SE, Rusfertide throttles erythropoiesis and elevates ferritin which is what we want.) [Info]
Rusfertide. Not yet approved. Currently in Phase III trials. Formerly known as PT-300. This is an injectable synthetic peptide. In PV patients, it was found that Rusfertide eliminated the need for therapeutic phlebotomy. This peptide is a human hepcidin mimetic (this detail will be important later). Rusfertide's structure is here. (Although PV isn't SE, Rusfertide throttles erythropoiesis and elevates ferritin which is what we want.)
Vamifeport. Abandoned. Ferroportin inhibitor. [Info] [Full review]
Sapablursen. Binds TMPRSS6 mRNA to block translation, increasing hepcidin. Not yet approved. Currently slated to enter Phase III trials in 2026.
Supplements
Cayenne. Didn't work.
Ginger. Did not make a difference in erythrocytosis in guys taking it.
Maca. A perennial plant (Lepidium meyenii) that grows in high altitudes of Peru. "Red maca reduced hemoglobin levels only in highlanders with abnormally high hemoglobin levels." [Source]
Garlic seems to stimulate RBC production independently of erythropoietin. [Source] The jury is still out on this one.
Aspirin and Nattokinase can be taken to avoid cerebrovascular events. They don't play a role in managing hemoglobin or hematocrit, they are for prevention. I don't know if they play well together.
You can take every other day Aspirin in an 81mg dose. I want to repeat -- aspirin does NOT lower your hemoglobin or hematocrit, but it can help prevent adverse cardiovascular events because it inhibits thromboxane, which promotes platelet aggregation. [Source] Aspirin's effect on platelets lasts the life of the platelet, or 10 days. Daily Aspirin over 81mg is too much, and some would argue even 81mg daily is also too much and every other day is better. Your body is always making platelets of course, but stopping daily Aspirin means the effect tapers off, it doesn't stop right away. Stop regular Aspirin a week before you go and give blood. Too much Aspirin in your blood and you could find yourself giving blood and still bleeding six hours later after you are done and bandaged. No joke.
Supplements you should AVOID when managing erythrocytosis
Ashwaganda increases "both the red blood corpuscles (RBC) and hemoglobin count." [Source]
B-12 and Folate can increase erythropoeisis, so let your source be dietary. Don't add more in a pill. And for Christ's sake do NOT do B12 injections.
N-acetyl-cysteine (NAC) "increases intracellular reduced glutathione, decreasing reactive oxygen species and enabling EPO production." [Source] Experience, both personal and in the discussion group, illustrate that using NAC does increase RBCs at a faster rate.
I read aerobic exercise helps.
This is true; exercise induced hemolysis reduced red blood cells. [Source]
Recommendation if you don't do phlebotomy: use Telmisartan and L-Citrulline. Consider quercetin (stronger than naringen) for lowering H&H, and understand quer and nar both lower ferritin. Consider nattokinase if you run high (clot issues? Clear the natto with your doc).
If you got here via a direct link, there is a 'managing without phlebotomy' section above this one.
Managing With Phlebotomy
There are people who say to never donate. Why?
Some think that if they don't have symptoms, then no one will have symptoms. They may say "my hematocrit is at 54% and I never feel anything. Therefore, NO ONE feels anything, ever, at any level. High HCT can be ignored because I ignore mine. Literally everyone is exactly just like me."
I mean, I'm not diabetic -- that means no one needs to inject insulin. Makes sense, right?
They also believe that cardiovascular events simply cannot occur because of secondary erythrocytosis. The science on this one says "maybe."
Most don't realize that the studies they look at on Pubmed didn't control for phlebotomy. The studies looked at men on TRT and their hematocrits and some of those men WERE DUMPING BLOOD.
"Wait. You're telling me that they studied whether men on TRT need to donate blood, and they were looking at guys who DID donate blood, and saw they had normal hematocrits?"
YES. THAT IS WHAT I AM SAYING.
I read a study showing that phlebotomy doesn't help.
No you didn't, because that's not at all what the study says. The study observed that of repeat donors on TRT, 44% had persistently elevated hemoglobin levels at subsequent donations. They reached the conclusion that "repeat blood donation was insufficient to maintain a hematocrit below 54%."
That makes about as much logical sense as "repeatedly filling your car's gas tank is inufficient to maintain a full tank."
Donors are on TRT. That's why they donate repeatedly. No one on TRT ever said that blood donation will maintain hematocrit below 54%. No one. Ever. TRT raises it, and you have to repeatedly donate, so why would anyone think donating would permanently solve the problem?
Someone in a FB group says you rebound faster after donating.
People not on TRT do, that's true. (The reason is due to erythroferrone.) Those of us on TRT are already in permanent rebound because our EPO is always elevated. To repeat myself: if you are on TRT, you are ALWAYS in "rebound mode."
Someone in a FB group says your RBCs are back where they were a week after donating.
This is a new one that started popping up in 2024. Get your own labs and see how full of shit this claim is.
Ultimately, when to donate (or ask for therapeutic phlebotomy) is up to you and your doctor working together. You can have a need to donate and not feel any symptoms.
Will my doctor order me to stop TRT if my hematocrit gets too high?
As of this writing in 2025, two guidelines cite stopping TRT at or above a HCT of 54. It doesn't matter whether it's true so much as this is what some doctors choose to go by for liability.
• the Endocrine Society May 2018 Clinical Practice Guidelines (the most current), state that clinicians should "Check hematocrit at baseline, 3–6 mo after starting treatment, and then annually. If hematocrit is >54%, stop therapy until hematocrit decreases to a safe level; evaluate the patient for hypoxia and sleep apnea; reinitiate therapy with a reduced dose." [Source]
• the European Association of Urology (EAU) Guidelines state that "if testosterone is prescribed then testosterone levels should not exceed the mid-normal range and the haematocrit should not exceed 0.54%. Testosterone dose adjustment may be required and/or venesection (500 mL) should be considered and repeated if necessary, if the haematocrit is greater than 0.54%. The haematocrit value of > 54% is based on the increased risk of cardiovascular mortality from the Framingham Heart Study, which was recently confirmed in another study." [Source] NOTE! The Framingham Study [source] examined high hematocrit and the risk of cardiovascular disease -- in smokers and NOT Testosterone users -- and did NOT reach a conclusion. Does that seem like a good study to base Testosterone dosing on?
Canadian Guidelines just quote these other two. [Source]
Do I donate whole blood or do I do this 'Power' or Double Red donation?
A hematocrit of 50 means your blood is 50% red cells, and the rest is plasma (49.5%) and white cells and platelets (about a half percent).
Donating double red takes twice as much of only red cells than whole and gives you your plasma back. It's actually based on your weight, FDA guidelines limit collection to ~15% of donor blood volume.
Donating whole blood does not change your hematocrit until 1 or 2 days post-donation because you are taking red cells as well as plasma and not changing the ratio of reds to plasma. Your body takes that long to replace your plasma. Donating double red replaces the plasma AND gives you saline to replace the red cells. Your ratio has changed during the process and hematocrit drops as the procedure is conducted.
Days between regular donations: 56, and you're taking plasma, whites, and platelets too
Days between double red donations: 112, and you're only taking reds
For a double RBC donation, studies indicate it takes 4 to 8 weeks (28 to 56 days) to restore the lost RBC volume in healthy donors. Speed depends on your EPO level.
If you do double, remember that your doctor can still order phlebotomy if you need it. Don't let the "I have to wait 112 days" freak you out.
I am going to repeat that because it doesn't seem to sink in with some guys.
If you do double, your doctor can still order phlebotomy if you need it. "But I'll crash my ferritin!" Who cares, we can fix that now.
The drugs in your body like Testosterone are in plasma, by the way. When you donate whole blood, you are passing Testosterone in your blood to donors (not that it's a big deal, but it gets asked about a lot).
Here is a calculator that will also tell you your blood volume. Here is a study on donor motivation. So you do it for the free keychain. [Source]
If you can't donate because you got blacklisted / you're flagged / you're gay / you like prostitutes / it's too far / etc
If you cannot donate and want to do it at home, you need a home phlebotomy kit and a friend who is a phlebotomist, or a nurse, or an EMT-Intermediate or EMT-Paramedic. Yeah, I know you want to do it by yourself. I just can't recommend it.
Could low ferritin be making me feel bad?
Yes, remember that starting TRT can lower ferritin... But if you only started to feel bad when your HCT got to 55, then the HCT is the real problem. A ferritin at or below 30 seems to be a common "I feel like crap" number for most men on TRT. A ferritin of 50 to 70 seems to take care of most issues. Very few of us are able to get higher than 70, and if we do get higher, it tends to drop down to 70 quickly. I have no real understanding of why this is.
A guy on Youtube said low ferritin from donating is really why I feel bad!
Literally who the hell cares. It's fixable. We now know how to raise ferritin 30 to 50 points in about a week. If TRT docs gave a damn about this problem it wouldn't have taken a guy like me to publish a solution.
Should I tell Red Cross I am on Testosterone Replacement?
The person measuring your hemoglobin might ask you how it gets so high. Even though TRT is not against the rules, I suggest that you don't mention it.
On paper, donating blood while on prescribed TRT is allowed; in my experience, mentioning it is a great way to start a fight with the technician. They are not all professionals who understand TRT. And under NO circumstances should you say that you benefit from donating. That's a whole separate issue with them.
My story: a Red Cross tech noted that I have high hemoglobin and I volunteered that it's because I am on prescribed TRT. I guess she decided that she didn't like Testosterone users, because I was told to sit and wait until I could be interviewed by the site's Medical Director, who came and had me answer several pointless questions after which she re-took my vitals (think about why -- if she raised my BP, she could reject me for donation. I stayed calm). I'm telling you, it has happened to plenty of us. If they remark that your hemoglobin is high and you think they're 'fishing' for a reason, just say you're a smoker or that you snore.
During a different visit, I also once made the mistake of saying "I need to donate" and had to backpedal when a tech explained that they cannot proceed if donation is medically necessary. They are not allowed / licensed to perform any kind of therapeutic intervention. There may be a blood shortage, but never underestimate how satisfied someone can feel after telling a TRT user to fuck off. We are lower than dirt to some of these people.
If you completely skipped Part 1, I recommend that you read it at some point.
The Vorck TRT Ferritin Protocol Simple Version Revision 4
You need:
• to be on Testosterone or have erythrocytosis from something (smoking, PV, sleep apnea, ideopathic secondary polycythemia, etc)
• to have RBCs over 5.5 for men and women
• to regularly have a hemoglobin of 16+ for men and women (you can dip if you donate but keeping your ferritin relies on a high HGB)
This won't work if:
• you have a Roux en Y gastric bypass which will cause iron supplements to bypass the body's sensing area in the gut
• you have C282Y hemochromatosis (H63D is ok)
• you have thalassemia (of any type)
• you are a normie who has iron deficiency and aren't on TRT. Seriously, this protocol is for people with a hemoglobin of 16 or higher.
Maybe won't work:
• You are on a "GLP" drug like Semaglutide, Tirzepetide, Cagrilintide, or Retatrutide. These all dramatically slow gastric emptying. Your iron pills will hit at all the wrong times. However, I had a user on Tirzepetide report zero issues.
You must:
• avoid supplementing vitamins C and D during (stop D one week before and during your protocol run)
• avoid a lot of heme iron. Eating red meat and some foods like oysters facilitates non-heme absorption. The best results come from low iron foods like protein powder, chicken
or turkey breast, white fish (cod, tilapia), canned tuna, salmon, pork.
I need you to repeat ten times: "He is telling me to take iron, but it will NOT be absorbed."
We are using the body's iron sensing mechanism to raise a hormone (hepcidin) and block the iron which, after day 1, goes into your sewer system.
Read the long version to understand why.
THE PROTOCOL
How to raise ferritin, the short "just tell me how" version
Three 70mg doses per day of Ferrous bisglycinate chelate spaced apart at 9am, 3pm, and 9pm to midnight all on the same day, at least 5 days in a row (most guys are doing 7 days as of Sept 2023). 70/70/70 every day for five, six, or seven days. You can be a little loose on the times (8am or 10am is fine, 2pm or 4pm is fine.)
9am
• Ferrous bisglycinate chelate, 70mg (I use Kirkman or Thorne or NOW brands but any trusted brand will do)
3pm (same as 9am)
• Ferrous bisglycinate chelate, 70mg (I use Kirkman or Thorne or NOW brands but any trusted brand will do)
9pm to midnight (same as 9am and 3pm)
• Ferrous bisglycinate chelate, 70mg (I use Kirkman or Thorne or NOW brands but any trusted brand will do)
Yes, all three are the same.
Net effect: daily iron overload of 210mg to 240mg triggers elevated hepcidin. You do NOT absorb the iron.
THE IRON IS BOOSTING HEPCIDIN. HEPCIDIN CAN ACT LIKE AN IRON DRAINPLUG.
YOUR FERRITIN (TRAPPED IRON) RISING IS FROM YOUR OWN RECYCLED RBC IRON.
When you're done -- stop, get your ferritin test.
Do NOT take an iron pill that is "slow release" to kick this off (you need an initial 'hit' of a lot of iron all at once). Do NOT take a 'combo' iron pill that has extra vitamins in it like C, D, B12, whatever. Just take a plain non-heme iron pill (most iron pills are non-heme. No meat sources). Just above 70mg please. I have used:
Klaire Labs and
Kirkman both 5mg AND 30mg and combine two of each for a total of 70mg (5mg, 5mg, 30mg, 30mg, is 70mg.Nutricost 36mg x 2 = 72mg
Getting timing or dose wrong means that you'll raise hemoglobin and have to donate again and your ferritin didn't even go up. "Don't be That Guy." Why non-meat? Heme iron doesn't boost hepcidin much, which is how this whole trick works.
If this didn't work. If you followed this exactly and your hemoglobin went up and your ferritin is unchanged, get checked for an HFE gene mutation such as for C282Y hemochromatosis (H63D is ok). Ancestry or checkiron.com is a cheap way to do this (example). So far I've had about 6 guys accidentally discover they have iron disorders (who tested and told me). (Relax, that's uncommon given the hundreds of guys who used this successfully.)
Another reason this might not work is use of GLP drugs.
Taking Semaglutide, Tirzepetide, Cagrilintide, or Retatrutide? These all dramatically slow gastric emptying. Your iron pills will hit at all the wrong times. If you know your delay in gastric emptying (calculating drug impact time using the facial flush reaction from taking a Viagra, I know that on Reta, my pills take 5 hours to hit), then you can do this. 9am becomes 4am, 3pm becomes 10am, and so on. But your rate of emptying may change by the time a week has passed.
Questions I get after guys read the short version:
Can I just ask a really stupid question? Why don't we want to absorb the iron? Because your hemoglobin will shoot right back up again.
So where is the iron in the ferritin coming from if we don't absorb the oral iron pills? Your body recycles 80% of its daily iron from RBCs, happening literally every second.
Why the weird times? Because we are mimicking hepcidin spikes that the body "expects." This is not well understood, but I can assure you that the times are a big key in making this work.
Can I use another kind of iron? My grandmother has ferrous fumarate / sulfate / whatever pills. Yes, but you need the right amount of elemental iron minimum which is 65 to 70mg. Read the back label to figure that out.
Can I take less than 70mg? NO. Less and your hemoglobin will go up, not ferritin! (60mg works but again, most makers are putting less in their pills.)
Can I take more than 70mg? YES. You bought a bottle of 36mg pills perhaps? That's 72mg — it's fine.
What happens if I go over 80mg? Well, I have a counter-question: do you enjoy shitting roofing tar? You can take more, but I don't recommend it.
Didn't this used to use 60mg? YES, but using a sensitive gram scale, I discovered manufacturers are putting less iron in their pills than they advertise.
Can I just take the pills once per day? NO. This won't work.
Can I take iron with food? Try to avoid this on days 1 and 2 when hepcidin is being driven up. Space two hours from food. The other days appear not to be so critical.
Are the times of day flexible? Technically, yes. But don't get creative here. You can do a first dose between 8am and 10am. Second dose can be between 3pm and 4pm. Third dose can be between 9pm and midnight.
Can I take heme iron instead of non-heme? NO. The reason is in the long four-thousand-word explanation further down.
Some guy said I need copper...? NO, you don't need to supplement it, but it won't hurt. I explain this in the long explanation below.
Dude I feel like freaking Superman the first two days I do this. Well technically the first day's dose does get absorbed. Hepcidin rises on day two. So you're feeling the effects of a massive dose of iron pushing serum iron up. It is most definitely temporary.
But ChatGPT and my anemic cousin say we need to take vitamin C? Damn it man pay attention. Did I not explain we do NOT want to absorb the iron. We just want the body to sense it, and raise hepcidin.
Can I take an iron pill with a bunch of extra shit in it like B12 and vitamin C or D? NO. STAY AWAY FROM "BLOOD BUILDER."
What about [supplement]? Guys, I don't know the effect of every supplement on hepcidin so I have to say please avoid anything in this list. And no, I don't know what Blackberry Extract or whatever does for ferritin. I'd like to, but I don't have the time to look them all up.
What do you have against vitamin D? Vitamin D suppresses hepcidin, so it would work against you here. A vitamin D3 pill has a serum half-life of 24 hours, but it converts to 25-hydroxyvitamin D which has a MUCH longer half-life. So daily D3 dosing gave you a constant level of D, which is why I say to stop your supplement a week before. Vitamin D from foods like eggs is not a serious issue because it's not enough to impact this. A 12-ounce glass of fortified milk typically contains about 150 IU of vitamin D which is not a big deal. The RDA daily is 600 units. I prefer you not go above that for the week before and during the protocol.
Didn't this used to be a 3-day process? Yes, when I first published. But gaining only 10 points of ferritin isn't worth your time. That's nothing. We tested 4 days, and then moved to 5. Most guys choose 7. We have several moving to 10 days.
What kind of result can I expect? Sample feedback: "I recently did your ferritin protocol and wanted to share my results. I am 36, been on TRT since 2018. My ferritin started to plummet since then (mainly due to blood donations every 2–3 months). The last time I checked, it was 10. However, I can't say I really felt low ferritin symptoms. Nonetheless, I tried your protocol last week. I used Iron bisglycinate, 75mg at 9am, 3pm, 8pm, for 7 days. Throughout this whole time I only ate egg whites, tilapia, tuna, whey, plain rice cakes. The result was great — my ferritin is now 94, and my Hb/Ht did not budge..."
I do this and only get 40 points myself. It varies.
How long will I keep my new ferritin level? I can pretty much guarantee you a month at least. You guys will get mad if I say it depends, so I will say that most guys with a hemoglobin of 15 or 16 will keep their level, plus or minus 3 points, for at least one month.
The Vorck TRT Ferritin Protocol Fully Explained Version Revision 4
How to raise ferritin, the long "I'm ready for technical details" full explanation version
Before I reveal the protocol again like I just showed above, let's step through some basics. If you don't have a medical or biochem background and you haven't already read the content from the first part of the page on elevated H&H, read Blood Basics and Iron Basics in Blood, Oversimplified. I will be re-explaining some key concepts from part 1 anyway in this part to make all of this easier.
TRT induces Iron Deficiency.
On TRT, hemoglobin is above 13, and ferritin is often low. This is technically "iron deficiency without anemia." The level of ferritin that qualifies as "iron deficient" is hotly debated. For our purposes, let's use a level of 50ng/mL (I will explain how I arrived at this later).
What are the symptoms of low ferritin?
Fatigue. Persistent tiredness and lack of energy, even after adequate rest, when other causes were ruled out.
Shortness of breath especially during exertion, not explained by lung or heart issues.
Heart palpitations.
Restless legs syndrome (RLS). Uncomfortable leg sensations and an urge to move them, especially at night.
Brain fog. Difficulty concentrating, memory issues, or slowed thinking.
Headaches or dizziness. Less common.
Tinnitus (ringing in the ears). Less common.
Additional reading: why can low ferritin be a problem and what does it feel like?
What ferritin level is ideal?
There is evidence that in women, a minimum level of 51 is where the body attempts to correct for low ferritin. No similar research exists for men that I am aware of, but for now that's a reasonable minimum target. [Source] I see an awful lot of guys on TRT not being able to keep numbers higher than the 70's. That's probably the TRT 'set point' for many of us. Remember that your blood test may show a 90 from running 7+ days but I cannot guarantee you'll keep that.
Ferritin: iron is stored in ferritin, a protein complex primarily in the liver, spleen, and bone marrow. Ferritin holds iron in a non-toxic molecular protein cage. A little bit of ferritin exists in serum. The liver's cells (hepatocytes) hold 80% of the body's ferritin and it is released as needed for red blood cell and hemoglobin production and other processes.
Ferroportin: this is a cellular protein that allows iron to exit cells when ferroportin's level is high, and traps iron in cells when ferroportin's level is low. Ferroportin is controlled by hepcidin.
Hepcidin: this is a single-purpose hormone that is the master regulator of iron in the body. Hepcidin decides when iron can enter the body via absorption and whether iron can exit cells (it does both simultaneously). When hepcidin is high, it binds to ferroportin, trapping iron in the cells (AND it blocks absorption of iron in the gut at the exact same time). When hepcidin is low, there is nothing to bind to ferroportin, so iron exits cells easily (AND it allows absorption of iron in the gut at the exact same time). Hepcidin is a cellular "iron drain plug."
Erythroferrone: this is a single-purpose hormone that is the master regulator of hepcidin in the body. It is produced by immature Red Blood Cells. Lots of new RBCs means your erythroferrone level is high. When erythroferrone is high, hepcidin is low (and from the paragraph above -- when hepcidin is low, there is nothing to bind to ferroportin, so iron exits cells easily.)
Eighty percent of your iron comes from your own recycled Red Blood Cells.
"Most of the body’s iron is bound to hemoglobin in erythrocytes. Iron from senescent red blood cells is recycled by macrophages in the spleen, liver and bone marrow. ... Most of the iron in the human body is associated with erythrocyte hemoglobin (~80%). ... As the circulating iron pool is comparably small compared to the daily iron demand, iron has to be continuously recycled from old red blood cells to reach the daily requirement of iron to maintain erythropoiesis and other bodily needs." [Source] This iron is what we're going to use for ferritin. We are literally going to divert it from hemoglobin by raising hepcidin and "blocking the iron drain plug" in liver cells.
A little bit of ferritin exists in serum. This amount in serum is reflective of tissue stores and is overflow. [Source] Ferritin in men tends to stay pretty constant for extended periods, weeks or even months.
On the other hand, serum iron is iron in the blood, and it changes hourly. Iron in the blood serum is going to get put to use primarily in hemoglobin and myoglobin. Serum iron varies in everyone from day to day -- that iron value on your "iron panel" blood test would have been different by dinner time. Iron is transported through the blood by transferrin.
On an iron panel, you will see a Transferrin Saturation Percentage (TSat%). That is a good indicator of your serum iron being released from cells. In normal people, it's between 20 and 45 to 50. TSat% can stay relatively steady over the course of a few days in some people.
If your TSat% is lower than 20% while fasting, you either have so little iron in the body that there's none to bind to transferrin, or hepcidin is high and restricting iron from exiting cells. Remember hepcidin's functions: prevent iron overdose and restrict iron from feeding pathogens. It isn't sophisticated enough to be able to "know" the difference between a flu virus and chronic arthritis. Inflammation goes up, hepcidin goes up, job done. More on this process is below, under "Ferritin also goes up when you're sick, on TRT or not."
If your TSat% is persistently higher than 55 while fasting, or goes high a lot seemingly randomly when you aren't supplementing, you have something wrong. You might have a disorder like hemochromatosis. We've had a few guys discover they carry hemochromatosis genes after reading this guide and getting tested. You can order a test from your doctor, but it's more expensive than Ancestry dot com which will also tell you.
What happens in iron overload? In iron overload conditions, such as hemochromatosis and thalassemia major, unregulated iron entry into the plasma overwhelms the carrying capacity of transferrin, resulting in non-transferrin-bound iron (NTBI), a redox-active, potentially toxic form of iron. [Source] When TSat% gets too high, that is what is happening. High circulating NTBI.
C282Y hemochromatosis: iron doesn't make hepcidin go up (now you see why this protocol won't work)
H63D hemochromatosis: the body doesn't make enough transferrin, so iron stays in serum longer, but ferritin can still build normally
For our purposes, it's best to think of serum iron and ferritin as opposites. Iron is either in the blood, or it's stored in tissue. That's not 100% accurate, but it's helpful to think of it this way.
On my protocol, we are going to block iron absorption (and trap iron in cells). I need to explain... Inhibited versus blocked iron absorption.
When research says such-and-such can "inhibit iron absorption and make you anemic," that means that iron didn't make it into serum which holds it until it is transferred to hemoglobin or ferritin.
- If you drank tea, the tannins bound with the iron and your body excreted that unabsorbed iron in feces. That is "inhibited absorption."
- If you took iron pills repeatedly, then hepcidin went up and your body blocked iron at the small intestine and also trapped iron in cells. That cellular iron is not available to be transferred to serum (via ferroportin) and will end up as ferritin. That is "blocked absorption."
Forcing iron to go into ferritin (rather than letting it go into serum, then hemoglobin) in normal people not on TRT is counterproductive because ferritin would drop like a rock in a pond after you finished your 5 days as your body stole all of the iron in the ferritin for use in hemoglobin. That's why a normal person with low hemoglobin would be foolish to follow this protocol.
You cannot 'take' ferritin, you can only make ferritin
Ferritin is an intracellular protein that binds to (wraps around) iron like a ball and releases that iron on demand in a controlled fashion. Ferritin is your iron bank account. You can't take bank account pills. There are some iron supplement pills on the market confusingly called "ferritin." Even if you consume animal organs (i.e. liver pills) to try to consume ferritin, your stomach breaks the protein down and it is treated as heme iron.
Ferritin comes in different types (isoforms):
H-ferritin (Heavy chain, FTH1). “Heavy” but stores less iron.
Has ferroxidase activity (converts Fe2+ or ferrous iron to Fe3+ or ferric iron for safe storage). Typically stores 500–1,500 iron atoms. Heavy has a less stable ferrihydrite core which allows for rapid iron release into tissue where it is found. These organs have the highest concentrations of heavy chain: heart, brain (sensitive to oxidative damage, H-ferritin helps detoxify Fe2+ rapidly), bone marrow (erythropoiesis requires rapid iron uptake for hemoglobin synthesis), placenta (rapid transfer to the fetus), kidneys, genitals, and the retina. (Other organs like the lungs are a mix of heavy and light.)
L-ferritin (Light chain, FTL). “Light” but stores more iron.
Has little or no ferroxidase activity. Typically stores 4,500 iron atoms. More prevalent in liver and spleen, where iron is stored long-term. Note that serum ferritin, which is secreted into the bloodstream, is mostly L-ferritin, with very little or no iron and little to no H-chain content.
This protocol is raising mostly ferritin in hepatocytes, or 'iron in the liver.'
That's good, but it isn't restoring ferritin to the many other organs that need their own local iron supply. Organs that need iron fast tend to be saturated with heavy chain -- that is the only type that can make iron available quickly because it has built-in ability to convert Fe2+ or ferrous iron to Fe3+ or ferric iron for fast use on export.
How ferritin is supposed to work in normal people NOT on TRT, vastly oversimplified
Joe, who is NOT on TRT, takes iron in a normal dietary dose, as well as a multi-vitamin, for a day's total ranging from about 18 mg to 30 mg per day. Joe has a hemoglobin of 14.9, so his body 'knows' that the iron doesn't need to push it higher. Transferrin transports this iron through serum. Hemoglobin normalizes, and everything functions well. If iron continues to rise, transferrin saturation (TSat%) reaches a peak (typically around 40% for most people) triggering an increase in hepcidin, and the body begins storing excess iron as ferritin that hour. [Source] Ferritin isn’t just a passive iron storage molecule, it's needed in all tissues, and that’s a much longer topic covered here: [Source]
When you're sick, and ferritin rises, the body has entered an inflammatory state where levels of cytokines, primarily Interleukin 6 (IL-6), are increased. This specific cytokine, IL-6, increases hepcidin which stores iron as ferritin even if your body needs it elsewhere. This is an evolutionary response where the body is trying to deprive pathogens of iron, necessary for the pathogens to survive. When the inflammation subsides, an elevated ferritin will fall unless your hemoglobin is high (like 17 or above). A prominent FB group calls this "falsely raised ferritin." As long as we understand the false refers to the raised part, it's as good a term as any.
If you crash ferritin while on TRT, ferritin is VERY difficult to raise it using conventional methods. Erythropoietin takes every bit of iron in the body and puts it into your blood. Suppressed hepcidin (from too much erythroferrone) means iron enters circulation whether you want it to or not. Iron is never withheld in cells to build or maintain ferritin. On TRT, all that iron in serum means hemoglobin can keep increasing past 17, 18, 19... the body never stores any extra iron you take as ferritin.
But I'm going to explain how to force the body to build ferritin.
The problem: TRT itself depeletes ferritin, and donating blood can crash ferritin
This is the possible double-edged sword when you donate: "hematocrit, hemoglobin concentration, ferritin, and red blood cell count (RBC), all key hematological parameters for oxygen transport, were lowered by a single donation and cumulatively further affected by the repetition of the donations. The maximal decrease after a blood donation was 11% for hematocrit, 10% for hemoglobin concentration, 50% for ferritin, and 12% for RBC." [Source]
There is ordinarily a "rebound effect" from repeated phlebotomy (where HGB gets worse faster), which does not happen in the presence of elevated hepcidin. [Source] Because my protocol elevates hepcidin, this rebound is eliminated if you do it right after donating / phlebotomy.
The solution: overpower erythroferrone by forcing hepcidin up
We need to leverage the iron blocking power of hepcidin to trap iron in cells for several days. We need an "iron drainplug" while the recycle iron from "dead" RBCs floods the metaphorical "bathtub" (in this case, the liver).
This obviously means that hepcidin will restrict iron availability for erythropoiesis ... and result in iron accumulation in tissue macrophages... Once [hepcidin is] bound to ferroportin, ... cellular iron export ceases." [source]
Raising hepcidin:
1. traps iron in cells of the small intestine (duodenal enterocytes) by binding to and degrading ferroportin and by inhibiting DMT1 transcription. [Source] DMT1 is expressed not only in intestinal lining, but also kidneys, and dendrites. We still don't know all of the locations. "This iron would be eventually lost [in feces] through the routine sloughing of enterocytes, which turn over approximately every 3 days in humans." [Source]
2. blocks iron release by liver cells (hepatocytes) by binding to and degrading ferroportin. Hepatocytes are liver cells, and 80% of the body's ferritin is the iron in these cells. [Source] [Source]
3. traps iron in certain macrophages also by binding to and degrading ferroportin. Macrophages are immune system cells that recognize and consume cell debris, viruses, bacteria, etc.
This last one is a big deal, because "FPN is abundantly expressed in reticuloendothelial macrophages of the liver, spleen, and bone marrow, [meaning] that this protein serves as an iron exporter in cells that recycle iron from senescent [aging] red blood cells." [Source]
In all of these cases, trapped iron cannot enter the blood. Elevated hepcidin means that this irontemporarily has nowhere to go, so hepcidin is "effectively shunting cellular iron into ferritin stores and preventing its absorption into the blood." [Source]
The major regulators of hepcidin blood levels are:
1.
iron status and consumption
2.
anemia
3.
hypoxia, and
4.
inflammation.
We will be using the first avenue, iron consumption, to raise ferritin.
I need you to repeat ten times: "He is telling me to take iron, but it will NOT be absorbed."
We are using the body's iron sensing mechanism to raise a hormone (hepcidin) and block the iron which, after day 1, goes into your sewer system.
This is the key to the whole protocol: you want to take an iron pill consistently so that you keep hepcidin elevated and every day the iron in the pill gets excreted, and the iron in the body from old RBCs is transferred to ferritin rather than going into your blood and elevating your hemoglobin (and hematocrit too).
But if you time it wrong, obviously, it will just make your high hemoglobin worse.
If there were a way to keep hepcidin high without taking iron, like injecting pure hepcidin subcutaneously, I would have you doing that instead. That's actually Rusfertide, which I discuss further down.
What kind of iron you need to use for this protocol
We use NON-heme iron only. I'll explain why in the next section on heme.
Before I explain how much iron to take in order to drive up hepcidin, I need to explain that the type of iron matters, because the actual amount of iron in a supplement varies a LOT. That 300mg iron pill is NOT really going to give you 300mg of iron.
There are multiple iron compounds available for supplementation over the counter, and they each yield different amounts of elemental iron. Below are some of the common forms and conversion to elemental iron:
• Ferrous Sulfate - Contains 20% elemental iron
• Ferrous Gluconate - Contains 12% elemental iron
• Ferrous Fumarate - Contains 33% elemental iron
• Polysaccharide-iron complex - Contains 46% elemental iron
• Ferrous bisglycinate chelate - Amounts vary on the formulation
• Iron citrate - Amounts vary on the formulation
Example: 325 mg of ferrous sulfate yields 65 mg elemental iron (i.e. 325 mg * 0.20 = 65 mg elemental iron). You can usually verify "elemental iron" on the product label. [Source] Some labels on the back just say "iron" without the word "elemental" though. The back label of an iron supplement bottle often states the actual iron content.
For bisglycinate check the back of the bottle for elemental weight.
Important point: I suggest that you buy ferrous bisglycinate chelate over the other types because we have a lot of experience with it. As a bonus, it is not affected by foods such as tea, which is famous for binding to iron and making it useless. [Source] We want the body to sense the iron and block it, not have tea interfere. You can use other types of non-heme iron if you want, but you have to use 70mg elemental iron no matter what type you buy.
Do you HAVE to use bisglycinate? No. In second place, some guys have used Ferrous Sulfate with success too -- users have used 325 mg ferrous sulfate pills (really 65mg per pill) to do this. These users report fewer gastric side effects. This is 65mg but will work. I say 70mg because manufacturers are putting less iron in their pills than advertised. If you have 65mg in a single ferrous sulfate pill, it's probably fine.
Make sure your pills DO NOT have added other vitamins! No "slow release" iron either for a first dose! You need to have a 65mg to 70mg 'hit' delivered all at once like a bomb to boost hepcidin. Slow iron might work for the other days; I have no idea.
We do not use heme iron from meat or heme pills for this protocol
You can't use iron from meat for this. Meat is heme iron and is RAPIDLY absorbed by the body. [Source] This is an issue with ferritin boosting; you need to use a non-heme (vegetarian) iron pill. Heme iron doesn't appear to boost hepcidin [Source] (There are issues with this particular study but let's not lose focus here.) It's easy to use non-heme pills. Here is what I buy at Amazon, I do not get paid for referral, 5mg version here. I do two 30's and two 5's for my 70mg.
Bisglycinate chelate is confirmed to use the non-heme absorption pathway.
If you click the More Details Dropdown, you'll see why "just eat more red meat" is counterproductive.
Heme iron (from meat) is absorbed intact via a specific transporter called HCP1 (Heme Carrier Protein 1) in the small intestine. Once inside the enterocyte (intestinal cell), the heme molecule is broken down by heme oxygenase to release Fe2+ (ferrous iron). This iron enters the labile iron pool and is exported into circulation by ferroportin. Heme iron bypasses the DMT1 (Divalent Metal Transporter 1) pathway that non-heme iron uses, which is more tightly regulated.
Non-heme iron absorption is more variable and more directly sensed by the body, triggering greater hepcidin response when iron levels are adequate. We rely on hepcidin response to build ferritin from trapped RBC iron!
Because heme iron is absorbed via a "low-regulation" route, the body doesn’t perceive it as a threat to iron overload the same way, and hepcidin isn't substantially raised. In addition, heme iron is more efficiently absorbed (~15–35%) and more bioavailable than non-heme (~2–20%). That's bad from a raised hemoglobin standpoint.
After you take non-heme iron, hepcidin starts to circulate in the blood. Hepcidin acts principally on transmembrane glycoproteins ferroportin (FPN) and divalent metal transporter (DMT1). When it does, this temporarily prevents iron export in all cells that express FPN and DMT1. Trapped cellular iron is what we want.
Read more on the role of hepcidin, ferroportin, HCP1, and DMT1 protein in iron absorption in the human digestive tract.
THE PROTOCOL
Three 70mg doses per day of Ferrous bisglycinate chelate spaced apart at 9am, 3pm, and 9pm to midnight all on the same day, at least 5 days in a row (most guys are doing 7 days as of Sept 2023). 70/70/70 every day for five, six, or seven days.
9am
• Ferrous bisglycinate chelate, 70mg (I use Kirkman or Thorne or NOW brands but any trusted brand will do)
3pm (same as 9am)
• Ferrous bisglycinate chelate, 70mg (I use Kirkman or Thorne or NOW brands but any trusted brand will do)
9pm to midnight (same as 9am and 3pm)
• Ferrous bisglycinate chelate, 70mg (I use Kirkman or Thorne or NOW brands but any trusted brand will do)
Yes, all three are the same
Net effect: daily iron overload of 210mg to 240mg triggers elevated hepcidin. You do NOT absorb the iron.
THE IRON IS BOOSTING HEPCIDIN. HEPCIDIN CAN ACT LIKE AN IRON DRAINPLUG.
YOUR FERRITIN (TRAPPED IRON) RISING IS FROM YOUR OWN RECYCLED RBC IRON.
When you're done -- stop, get your ferritin test.
Do NOT take an iron pill that is "slow release" to kick this off (you need an initial 'hit' of a lot of iron all at once). Do NOT take a 'combo' iron pill that has extra vitamins in it like C, D, B12, whatever. Just take a plain non-heme iron pill (most iron pills are non-heme. No meat sources). Just above 70mg please. I have used:
Klaire Labs and
Kirkman both 5mg AND 30mg and combine two of each for a total of 70mg (5mg, 5mg, 30mg, 30mg, is 70mg.Nutricost 36mg x 2 = 72mg
Getting timing or dose wrong means that you'll raise hemoglobin and have to donate again and your ferritin didn't even go up. "Don't be That Guy."
If this didn't work. If you followed this exactly and your hemoglobin went up and your ferritin is unchanged, get checked for an HFE gene mutation such as for C282Y hemochromatosis (H63D is ok). Ancestry or checkiron.com is a cheap way to do this (example). So far I've had about 6 guys accidentally discover they have iron disorders (who tested and told me). (Relax, that's uncommon given the hundreds of guys who used this successfully.)
Another reason this might not work is use of Semaglutide, Tirzepetide, Cagrilintide, or Retatrutide. These all dramatically slow gastric emptying. Your iron pills will hit at all the wrong times.
Where does 70mg come from?
"An oral load of 65mg of iron in healthy volunteers caused >5-fold increase in hepcidin within 1 day. ... The assays established that hepcidin transiently rises 4-8 hours after oral iron administration and that it is subject to diurnal variation with a midday maximum, perhaps because of dietary iron ingestion." [Source, source, source]
60mg and up works, but I found that manufacturers are putting less iron in pills than advertised.
Do I need to space the iron from food?
On Days 1 and 2, yes, space your iron two hours. I want you to expose your body to a lot of iron at once. The other days appear not to be so criticial.
Taking iron with food introduces a complex matrix of nutrients, which may dilute or bind iron, potentially affecting local iron concentrations in the duodenal lumen. Taking iron on an empty stomach results in a higher local concentration of iron in the duodenum, as there’s no food mass to dilute or interact with it.
Are the times flexible?
Yes but not by much. You can do a first dose between 8am and 10am. Second dose can be between 3pm and 4pm. Third dose can be between 9pm and midnight.
The times come from research showing that hepcidin levels trend upward during the day. That's probably due to ingestion of food, but I can assure you that other tested times do not work, I tried multiple variations including a twice daily routine. If I had to point to a justification for the times, I wouldn't be able to. All I can say is that we are emulating the natural cycle of hepcidin, boosting it at it's low points or when it starts to drop, and that it seems to work.

When do I start the protocol?
You can do it ANY TIME as long as your HGB is 16 or higher. Most guys do it around blood donation which is logical. I asked my hematologist if I should do this just the week before donating. He suggested right after donating would be better, because it overrides erythroferrone (but we're already flooded with it anyway, being on TRT). If you donated at noon for example, you can even start my protocol on the same day at the 3pm dose if you want.
Stay faithful; you cannot miss a dose in this for the first 2 days, but if you miss a single dose on day 3 or 4 or 5, it's not a big deal at that point.
Explain the dietary concerns?
I get asked about foods. I eat boring foods when I do this protocol, like protein powder or tuna, that kind of thing. You can use this tool to find low C and then match results with low D foods I suppose. Avoid a lot of heme iron. Eating red meat and some foods like oysters facilitates non-heme absorption. The best results come from low iron foods like protein powder, chicken
or turkey breast, white fish (cod, tilapia), canned tuna, salmon, pork. A steak is only 6mg of iron but the problem is that the meat stays in your gut, facilitating iron absorption. Does it increase absorption of non-heme iron, research doesn't give a clear answer.
I want to do it again. How long do I wait?
I am concerned that you make sure you didn't elevate hemoglobin. First timers should make sure it worked before running again. For you regulars, I used to say wait 2 weeks. I really had no basis for that, I just wanted to play it safe. When you stop, you have iron from your last day in your gut cells (entocytes). The body sheds them after three days. So technically when you stop, you have 2 days where iron pills you took on your last day can absorb. That's a constant. So waiting 3 days or 7 or 14 doesn't matter -- you want to go again, go ahead, no waiting is needed.
How long can I expect to keep my new ferritin level?
I can pretty much guarantee you a month at least. You guys will get mad if I say it depends, so I will say that most guys with a hemoglobin of 15 or 16 will keep their level, plus or minus 3 points, for at least one month. Many are keeping it until their next donation, but don't hold me to that. We all do different amounts of Testosterone, and have different levels of Serum Test and EPO, and therefore different amounts of ferritin slipping out of cells. Personally, I have a trough T level of 750-800ng/dL and I lose about 3 points of ferritin per month.
A note on doing a "Vorck Iron Blast"
Some guys don't care about a higher ferritin and want to feel GREAT and not raise their hemoglobin either. You would do my protocol for 3 days. I really don't suggest that and don't see the point, but I do know some guys do this to feel awesome and get that "new iron load" feeling.
A note on being trans / on GAHT
This entire process works the same for F to M transitioners.
When posting questions in my FB Iron group please point it out though. Your Estradiol can complicate things and it's important to know if the process fails.
Things that work against raising ferritin (only DURING the protocol)
Elevated Estrogen. "This has been attributed to the ability of estrogen to suppress hepcidin synthesis, maintain ferroportin integrity and enhance iron release from iron-absorbing duodenal enterocytes and iron-storing macrophages and hepatocytes." [Source, Source, Source] Note that women with normal levels of Estrogen have lower levels of hepcidin; this link disappears after menopause. [Source] Estrogen lowers hepcidin and makes ferritin difficult to build, prioritizing hemoglobin. [Source]
Do NOT go too low on your Estradiol level
You need E2 for your bone density. Many in the anti-Aromatase Inhibitor crowd actually believes, incredibly, that AI users are attempting to get their E2 to zero. (I'll give you all a minute stop laughing at the anti-AI crowd.) The question is, WHAT minimum levels of E2 are needed to prevent bone density issues?
From Aromatase Activity and Bone Homeostasis in Men by Luigi Gennari, Ranuccio Nuti, John P. Bilezikian
"A review of several studies showing that in most but not all cases, elimination of Estradiol using AIs negatively impacts Bone Mineral Density... The data argue that men need a sufficient concentration of estrogen, defined as a threshold value, for normal skeletal remodeling. In all of these studies, the required concentration of bioavailable estradiol appears to be remarkably similar, ranging from 10 to 14 pg/mL."
Normal bioavailable E2 is 21 to 38 pg/mL. 2 to 3% is bioavailable and 3% corresponds to a serum total of 41 to 75 pg/mL.
The minimum required concentration of bioavailable E2 is 10 to 14 pg/mL and 3% corresponds to a serum total of 20 to 28 pg/mL. In other words, having an E2 below this minimum level presents a risk to bone density.
What's a healthy E2 level? This formula gets used a bit. It is set up to use the most common units that people quote their lab values in.
E2 in pg/mL divided by Total Testosterone in ng/dL should be between .03 and .1
For example: E2 is 60, Total Test is 600, this ratio is therefore .1 and so this E2 should not be causing symptoms of high Estrogen. Maybe check other factors before using an AI.
Second example: E2 is 133, Total Test is 1,100, the ratio is .12 and so it is possible that if you have symptoms, your E2 might be causing those symptoms.
Third example: E2 is 18, Total Test is 850, the ratio is .02 and it would not be a surprise if you had zero libido because of this low Estradiol level. Elsewhere on the page you'll see using Icariin to raise E2 indirectly by upregulating Aromatase.
Estrogen needs to be high and other lies
I am not anti-Estrogen but people aren't being told the truth by the TRT users who are 20 years behind and advocating high Estradiol.
A woman's body, during pregnancy, raises Estrogen to create more RBCs and put them into hemoglobin because the maternal blood load and O2 needs to be high. That doc on Youtube that goes on and on and on and on and ON about the benefits of E2? Did you ever read the E2 levels in the studies he flashes on the screen? No? Maybe ask yourself why he's touting the benefits of Estrogen when those benefits are highest at pregnancy levels. Yes, E2 is neuroprotective. Great! But is it really smart to have an E2 so high that you get erectile dysfunction just in case you get into a car crash and need the neuroprotective benefit?
"But Estradiol is an intracrine hormone!"
Yup. It is. So what? Oh, were you about to make an "argument" that using an AI reduces Estradiol in tissues and that's the literal end of the world? Were you going to say stuff about tissue biopsies to figure out the E2 levels you need? Different tissues express different amounts of Aromatase, and serum E2 corresponds to Free Estradiol. Yup, Free E2 is a 'thing' just like Free Testosterone. (And I suppose we need tissue biopsies to see if we need to inject a higher dose of Test too, right?) There goes the 'biopsy argument,' if you can even call it an argument.
"But AIs are approved for cancer! Therefore, they are bad!"
Your Uncle Arthur's Methotrexate that he takes for his arthritis was approved for cancer first.
Vitamins C and D lower hepcidin for several hours, and we want to avoid that, so don't take C or D supplements while you are trying to raise hepcidin to restore your ferritin level. I'm not saying don't ever take them, I'm saying skip them while you're working to restore ferritin. [Vit D lowers hepcidin] [Vit C lowers hepcidin] Vitamin D takes 2 days to clear from your system. Spending time in tanning beds or outdoors in intense sunlight may invalidate this protocol. UVB creates Vitamin D, as much as 15,000 IU in a 15 to 30 minute time span. I've had two reported failures in the protocol due to sunlight exposure and tanning bed use.
The metabolites of vitamin D, Calcidiol and Calcitriol, suppress hepcidin by binding to the vitamin D receptor (VDR) in hepatocytes and other cells. This leads to downregulation of the HAMP gene, which encodes hepcidin.
Drinking alcohol during the protocol. [Source] There are multiple studies on how alcohol lowers hepcidin, but the magnitude is hard to pin down. Any alcohol downregulates hepcidin. Binge drinking really craters it. So, out of diligence, I am recommending you not drink for your 7 day protocol run.
Supplements I tried to raise ferritin other than iron
Adenine - doesn't work. Adenine is a known strong hepcidin agonist. [Source] Adenine is sold as a supplement and is sometimes incorrectly called Vitamin B4. There is a bulk chemical supplier selling it on Amazon. A lot of hits will come up for NADH. It actually isn't the same thing. I grabbed toxicity info from a 1940's study that was the best one I could find (and remember, I have full access to the National Library of Medicine.) I tried 400mg per day split up at "the iron times" for 5 or 6 days and it had zero effect on my ferritin. Dr. Tomas Ganz (I wrote to him) said you would have to take a "kidney-killing" dose.
Capsaicin - Capsaicin administration significantly increased hepcidin levels in a rat study. [Source] Unfortunately 1 gram per day did not increase ferritin or lower hematocrit in myself or other testers.
Genistein - doesn't work. Apparently an Estrogen mimetic that is also a hepcidin agonist. 1 gram per day produced no rise in ferritin.
Icariin aka Horny Goat Weed - doesn't work. Icariin is a known moderate hepcidin agonist. 100mg per day for only a week (!!) raised my Estradiol from 40 to 70 though, and my Test was the same, so it wasn't a rising T level. Icariin upregulates Aromatase. [Source] If you overdid your Arimidex, perhaps this supplement would probably help you recover. Some Horny Goat Weed supplements are just crushed up plant with very little Icariin -- you have to be sure that what you buy has a significant amount of the active Icariin ingredient. People are asking me what brand I bought so here it is, Icariin from the seller. Amazon doesn't carry this one. Also a source of Icariin at Nootropics Depot too.
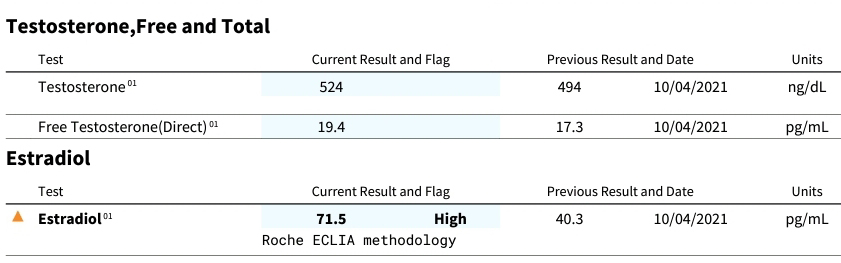
Melatonin - apparently it is one reason hepcidin goes up at night. [Source] The problem is that the half life of melatonin is 40 minutes max. So should you take it at bed time for my protocol? I would say yes, but should it be a lot, and should it be extended release? Probably. It doesn't last long enough. I have no specific recommendation right now. I tried 60mg every night, because you guys know me and I'm ridiculous, and got zero rise.
Omeprazole - doesn't work. The Proton Pump Inhibitor Prilosec (which increases hepcidin in mouse models [source] but apparently not in humans) has been found to reduce the need for phlebotomy in C282Y hemochromatosis. [Source] The problem is that in the human research it was found that "The mechanism of how PPIs influence iron metabolism seems not to affect hepcidin regulation but acts in the stomach and at cell level in the erythroblasts and macrophages." So it interferes with, but doesn't block, iron. It won't help for our protocol.
Turkey Tail mushroom - I took 5 grams (grams, not mg) three times per day for 5 days with the idea that it might elevate my IL-6 levels and promote hepcidin elevation. Well, my WBC count went up from 7 to 10.3, but my ferritin levels didn't go up. At least the WBC elevation matches research showing the immunity boosting property, but I'm not particularly interested in that personally. (Yes, I "could have" been sick, but in the few days between blood tests, I don't think so. I'm 'that guy' who gets CBCs all the freaking time.)
Supplements I tried to raise ferritin other than iron that have some effect
Sulforaphane - No major effect on ferritin while on my protocol (10 to 15 points maybe). This supplement upregulates Nuclear factor erythroid 2-related factor 2 (NRF2). From this study, "Nrf2 regulates iron metabolism pathway in response to oxidative and electrophilic stress by activating transcription of genes coding for ferritin heavy chain (Fth1) and ferritin light chain (Ftl) [109], thus increasing ferritin levels [110]. As a result, Nrf2 indirectly promotes iron storage and reduces the intracellular levels of redox-active free iron atoms. Moreover, Nrf2 also regulates labile iron (redox active, exchangeable and chelatable) by altering its transport across the cell membrane by up-regulating the expression of ferroportin. [Source] The BROC stuff I bought from Amazon
L-Citrulline - On paper, this builds ferritin by restricting the release of iron for use in hemoglobin. Along with Telmisartan, this 'froze' my H&H in place. Unlike turmeric, quercetin, IP6, etc it won't lower ferritin. More below.
Since hepcidin is a peptide, can it be bought?
Tricking the body into making hepcidin would be unnecessary if we could just inject it subcutaneously.
Rusfertide [link, link], a mimetic, is being trialed as a drug treatment for erythrocytosis conditions. Human hepcidin, compare to Rusfertide. They could make an identical molecular knockoff but then you can't patent something like that so they make a mimetic. Maybe one of the peptide makers can figure cloning this one.
Anyway, actual real-deal hepcidin is apparently available for purchase as a lab research peptide. You have to use the older terminology for it to find it: LEAP-1 (liver-expressed antimicrobial peptide), sometimes also called hepcidin-25. Because animal experimentation with this is common, you will have to hunt for the human variant. It's out there but it's hard to find. I'm not going to link to it because I have idea how to direct you to use it safely. It is unbelievably expensive.
Here's an odd thing about hepcidin: research has confirmed that this peptide has functionality across species. Zebrafish hepcidin works in mice. Mouse hepcidin works on monkeys and human cells in a test tube.
Show us a sample 5 day run
Here is a typical result. Remember, results depend heavily on following the protocol exactly for 5 days, and depend on your starting RBC load. Starting with RBCs at 4 won't have a good effect -- this whole process is driven by endogenous (your body's existing) iron, not exogenous (from supplements) iron.
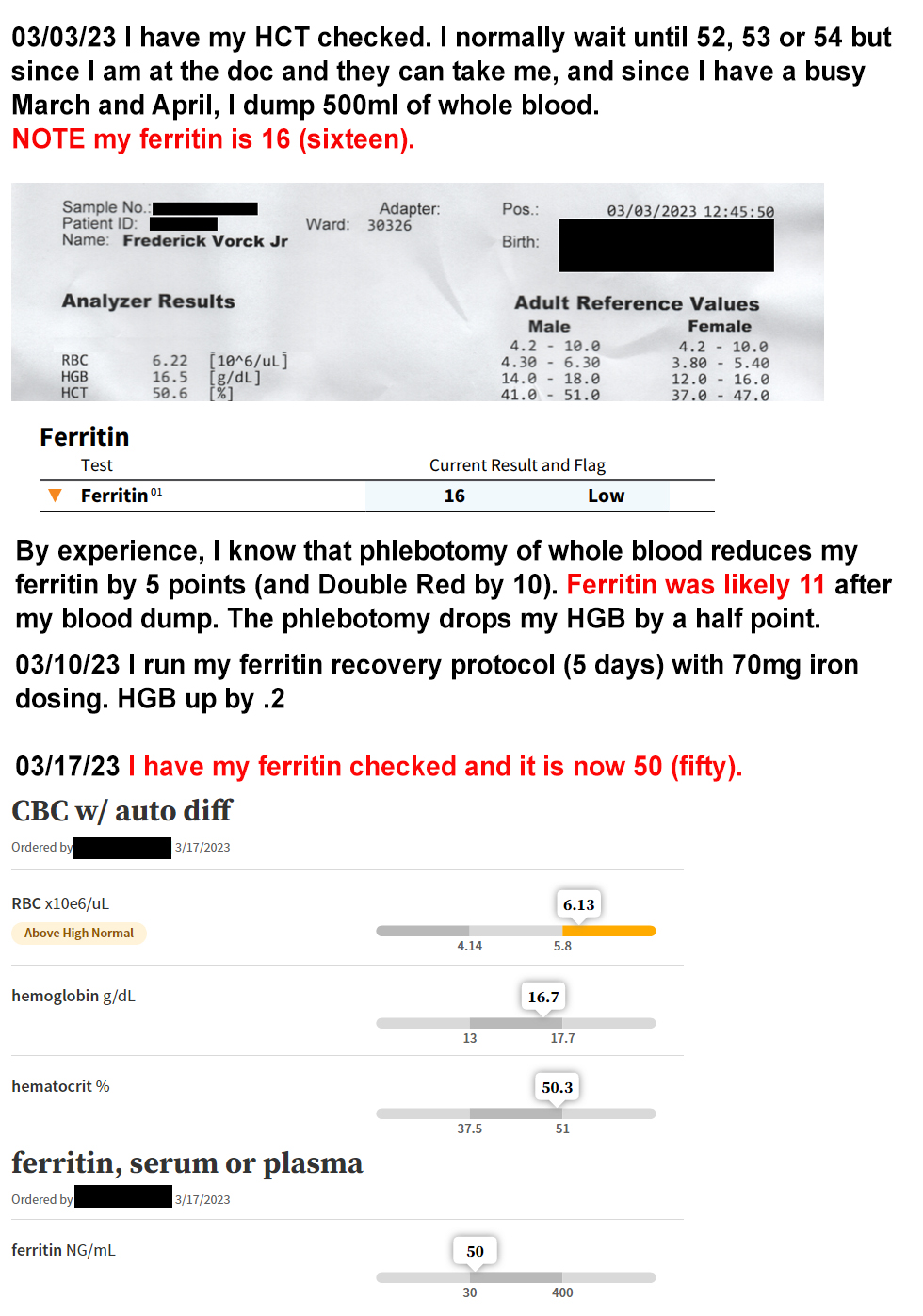
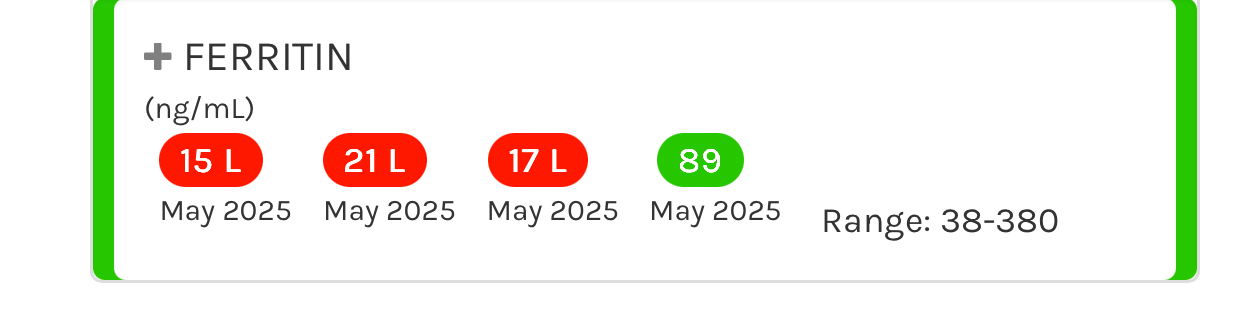
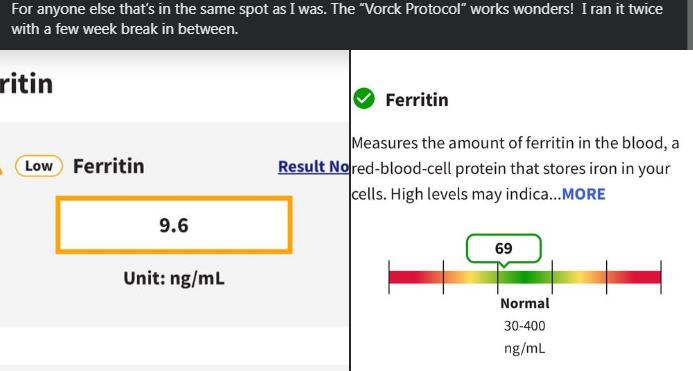
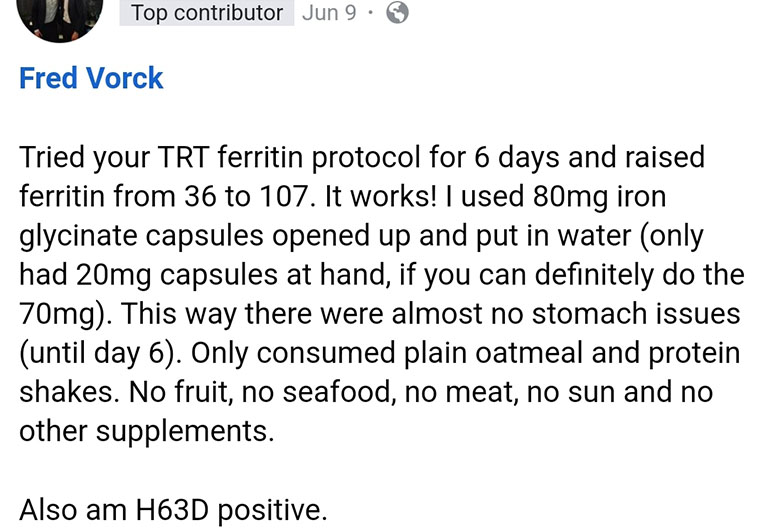
Summary
If you are on TRT, you have multiple options for controlling erythrocytosis and the resulting high hemoglobin and hematocrit:
- modified dosing to be daily, or daily with a lower overall dose.
- regular phlebotomy or donation, with ferritin rebuilding.
- drugs like Telmisartan or grapefruit extract supplements.
- consider, as applicable, CPAP treatment or smoking cessation.
Miscellaneous
Do you consult?
Not any more. It got overwhelming. I did $60 for one hour and now I just don't have time in my life. Sorry.
When doctors tell women and anemic men (who have hemoglobin levels of 13 or below) to take iron every other day, that’s because the hepcidin level is back down after 24 hours, so the iron will be absorbed into the bloodstream. [Source] They didn't even try to suppress hepcidin with Vitamin C or D in the study. Hopefully you the reader understand why the study conclusion is less than useful. (All they had to do was take Vitamin D and the iron blocking by hepcidin wouldn't have been an issue.)
We on TRT want high hepcidin for 5 days, though. For us on TRT, every other day iron dosing will raise hemoglobin and hematocrit and will keep ferritin low. That’s the opposite of what we want.
Remember from earlier -- think of iron in the blood as the opposite of ferritin.
The process of iron absorption in the gut. [Source 1, Source 2]
Could elevated hepcidin be a biomarker for some cancers? [Source]
The action of hepcidin in the context of chronic inflammatory disease. [Source]
Persistently elevated hepcidin (high ferritin, low HGB and RBCs) is a mutation in the TMPRSS6 gene. [Source]
This has been around since May 2021? Why am I hearing about this just now?
Because you spent time in the wrong online community. Trust me, I tried spreading the word. I got thrown out of groups and shadowbanned on Reddit. Blame your imbecile mods and brain dead filters.
A Reddit post actually referenced this which was what made me try to post, but alas, no luck.
Issues and Criticisms
Criticism: use of iron can raise RBCs (eventually when the ferritin drops again)
This one came via an April 2022 e-mail from Dr. Tomas Ganz, the MD who discovered the hepcidin peptide, after I asked him to review my protocol (yes, I really asked him about this). He acknowledged that raising hepcidin works, but he advocated using a mimetic like Rusfertide (because you absorb iron the first day). Obviously he's not wrong, but ... we can't wait for the FDA on this.
Criticism: does this use inflammation? Won't ferritin fall again?
Your new ferritin level will stay in place if you have a high hemoglobin and you follow the directions. We are not using inflammation. Hepcidin is an acute phase reactant, but it is raised via a few different methods. The iron administration pathway is separate from the inflammation pathway. [Source] You can change a light bulb using a step ladder or standing on a milk crate but you wouldn't say step ladders are the same as milk crates.
Criticism: not all the studies you use took place in TRT subjects
Some studies were on women, for example, or trans F to M. Some were on people with diseases, such as kidney disease. If the thing being discussed is true independent of these things, I use it. One example is Angiotensin II receptor agonists for SE. This was a finding in chronic kidney patients on dialysis. However, the drug clearly creates a blockade of erythropoietic effects of angiotensin II on red cell precursors. The dialysis aspect of the study doesn't materially affect what we're looking at. In addition, I have access to full studies through my healthcare institution, so just because a paper is paywalled doesn't mean that I relied on the summary alone.
Criticism: a few studies that you cite were on mice
The model of iron homeostatsis that we have developed has been found to be remarkably identical broadly across mammals. Hepcidin, it has been found, even works cross-species. Mouse hepcidin will actually work in other animals. Mouse experiments by and large mirror what happens in humans vis a vis iron and hepcidin.
Criticism: ferritin is bad and you need copper not iron...
GTFO with that Morley Robbins horse shit. My process WORKS. Go try your Root Cause garbage and see how much worse you feel with a ferritin below 20. Copper has a minor role in transferrin and ferroportin and the ferritin cage and does not MOVE iron in any way. We aren't even trying to absorb the iron.
Criticism: a guy on YouTube said...
The guys on YT talking about ferritin just make me laugh. One actually said low ferritin doesn't matter if serum iron is high. Serum iron changes hourly. That video was made by a group that's 20 years behind on TRT anyway. At a point, you get too far behind to catch up.
Criticism: this page goes really light on how iron works
I admit this page is shorter than I would like, but I have to strike a balance between explaining fully and explaining just enough to show why this ferritin protocol actually works.
Some people like videos so here's one showing how iron is processed. [Iron metabolism video]
Credits
My thanks
I leveraged studies and anecdotal data and received a LOT of help from Kyle Van and Keith R. You two have my sincere thanks.
Thanks to Doctor Ali who told me my info and ideas made sense and said "it could work" and encouraged me to go full bore when this protocol clearly did work.
Thanks to Jeremy M. for testing out various supplements and sending me info on drugs and supps that can lower HCT.
And of course thanks to Dr. Tomas Ganz who personally answered several key questions I couldn't find answers to online.
About the author
I started TRT in 2001.
My opinions are my own and not those of my employer.
Some loser who refused to click and read once asked what my credentials are. Like that guy, I'm pretty much a nobody. The difference is that I'm the one who reads all of the studies other people don't want to read.
For 20 years, I waited for someone to write about iron and donation issues surrounding TRT and how to increase ferritin.
And for 20 years, no one did.
So in January 2021, I did the research myself, I developed a protocol myself, I hired a hematologist myself (literally paid him to sit and listen to me talk for like 45 minutes), I tried my protocol on myself multiple times with different times, and in May 2021 I created this page.
Predicted Estradiol: pg/mL
Predicted DHT: ng/dL
This formulas are articulated in "The Effect of Injected Testosterone Dose and Age on the Conversion of Testosterone to Estradiol and Dihydrotestosterone in Young and Older Men," Journal of Clinical Endocrinology & Metabolism, 2010. They are:
Estradiol (pg/mL) = (138.3 × TT) / (1470.1 + TT)
DHT (ng/dL) = (260.4 × TT) / (2169.6 + TT)
Where
TT is total testosterone in ng/dL.
Result: ng/dL
Result: ng/dL
Also: pg/mL
Convert Estradiol from pmol/L to pg/mL
Result: pg/mL
Calculate Estradiol to Testosterone Ratio
Simple Ratio [E2 in pg/mL ÷ TT in ng/dL]: (percent uses E2 in ng/dL)
Flipped around [TT in ng/dL ÷ E2 in pg/mL]:
Please be aware that 1) there are multiple schools of thought on ratio, 2) symptoms or absence of symptoms matters and this isn't just about numbers, and 3) "no research exists on this for men on TRT!" also applies to injecting Testosterone more than once per week (yes, really).Nelson Vergel commentary on ratio.
Free & Bioavailable Testosterone Calculator
Free Testosterone:
Not-SHBG bound Testosterone*:
Percentage of Total That Is Free: %
This calculator is shamelessly stolen from the ISSAM Calculator and re-implemented by me. It uses the Vermeulen equation to estimate free and bioavailable testosterone levels based on total testosterone, SHBG, and albumin concentrations. Reference "A Critical Evaluation of Simple Methods for the Estimation of Free Testosterone in Serum," Journal of Clinical Endocrinology & Metabolism, 1999.
Most guys don't get Albumin drawn, and the 4.3 is a presumed conservative average.
* SHBG bound Testosterone is used. We've known since 2005 that SHBG transports Testosterone into cells expressing megalin. [Source]
Appendix
Iron related reading
Hepcidin and ferroportin interaction
Ferritin light chain, heavy chain, hemosiderin
Change log
May 2021 to August 2023, I made edits but didn't log them. A user asked me to start a changelog then. September 2023, added notes on DHT and Estrogen contributing to erythrocytosis. Added info on Telmisartan and notes about Losartan. Added 5a reductase inhibitors and Arimidex to the beneficial drug list. Added "notes on Estrogen." November 2023, notes that most users are doing 7 days. Added notes about stopping vitamin D for the week before the protocol as well as during. Minor note on ferroportin added. Note on semaglutide/tirzepatide added. Amlodipine added. December 2023, melatonin discussed. Feb 2024, Cayenne evaludated (didn't) work, ginger being trialed for controlling speed of RBC rise. March 2024, Mounjaro failure documented and gastric bypass notes added. March 2024, grapefruit / naringen is a chelator which is why it works. This can reduce ferritin too. July 2024 added statement on how long you wait before going again. Added Divesiran reference. August 2024 statement on alcohol throwing off the protocol. September 2024 Jeremy M. recommended Quercetin which has research support for lowering hemoglobin. April 2025 minor text revisions, added Hemoflow under supplements. Added L-Citrulline for reducing HCT. June 3, 2025 massive page overhaul, reformatting, added details dropdowns. Removed "take a small iron supplement every day" advice. Clarified L-Citrulline. July 2025 added my calculators and converters. September 2025 oops, I have "space your iron from food" in the short version but forgot to add it back into the longer protocol narrative after the massive page overhaul. Added it back.